Medical careers

Review status
Based on a medium-depth investigation
Table of Contents
Research process
Most of the data used in this profile was culled from national (e.g. Office of National Statistics, Bureau of Labour statistics) or international (e.g. OECD, WHO, WB) statistics, with supplementary data from polling agencies like Gallup. Relevant academic papers and studies were found mainly via Pubmed. I have also performed analysis on available data independently where appropriate, and (where data has not been available) drawn on my own experience as a junior doctor and informal discussions with my colleagues.
We have mainly focused on US and UK medicine, however, we believe the findings are broadly applicable across the developed world, and have marshalled international data where available to show various points likely generalize.
What is this career path
Medicine is a profession that demands a medical degree, either post-graduate only (in the US) or as an undergraduate degree (in the UK and Australia). Medical school takes 5-6 years.
After medical school there is a further period of being a junior doctor learning a particular specialty. In the US, this comprises internship and residency, with or without additional fellowships, and takes 3 or more years. In the UK there is a post-qualification foundation programme for two years, then training programs of 3 or more years. After this, one is a fully qualified doctor in a given specialty (e.g. general practice/family practitioners, cardiac surgeon, psychiatrist, etc).
What is it like day to day?
The daily life of medicine varies by specialty. A general practitioner or family physician will primarily work in the community in a clinic, whilst an internal medicine doctor will work in hospital. Some doctors will work primarily with chronic conditions and consequently work mostly ‘9 to 5’, whilst others like emergency physicians can expect to work frequent night and weekend shifts. Surgeons and anaesthetists will focus on practical procedures, whilst radiologists or histologists will be examining images or samples and may seldom see patients directly.
Why pursue a medical career?
Satisfaction
Doctors are among the most satisfied with their careers, but stress and burnout is significant problem.
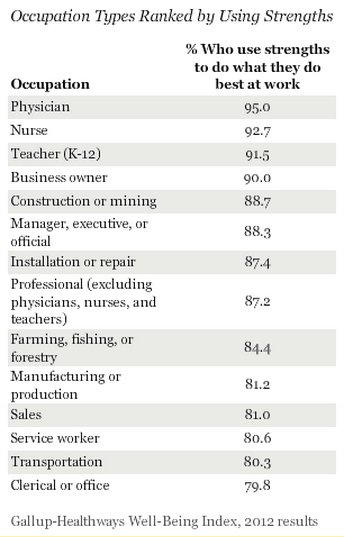
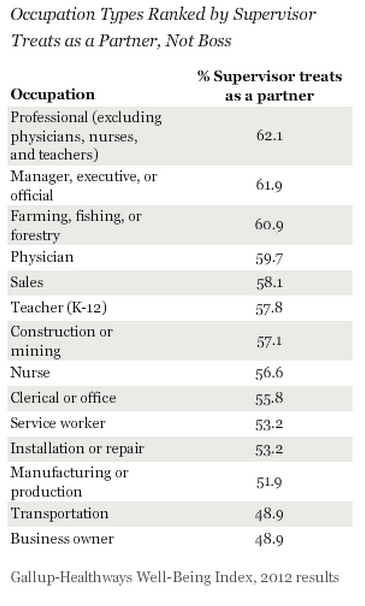
In the US, a Gallup poll in 2012 of 172600 adults places physicians first out of fourteen groups for general well being.1 Physicians still do strongly when restricting to measures of job satisfaction: they come first in percent satisfied with their job (95.5), first in “using their strengths” (self-actualization), and fourth in their supervisors treating them as a partner.2
The payscale salary survey also asks respondents in the US about satisfaction, stress, and how meaningful they find their work. Out of 454 occupations, physicians are in the top third by satisfaction, and the top tenth by how meaningful they find their work. The survey suggests significant heterogeneity within the medical profession: US surgeons are in the 95th percentile by satisfaction, US Obstetricians and Gynaecologists in the seventh.3 (For more, see this paper comparing many more specialties in the US).
In the UK, the Office of National Statistics directly collects data on life satisfaction, and the cabinet office has analysed this by occupation. When stratified by occupation, medical professionals came seventh of 274.4 Unlike the Gallup poll, there was no direct ‘job satisfaction’ measures; it was not necessarily the nature of their work that grants UK doctors increased levels of life satisfaction.
Despite this generally rosy picture, there is significant concern within the medical profession about physician stress and burnout. The payscale survey has physicians in the top fifth of professions by stress5, and a study comparing US physicians to the general population show them to be at significantly higher risks of burnout and of being dissatisfied with their work-life balance.6
Earnings
Doctors are amongst the highest paid of all professions. Compared to other high paying careers, their pay has low variance: whilst they reliably earn a lot of money, it is very rare for a physician to earn several times the median (cf. finance, or entertainment, where the ‘superstars’ can earn orders of magnitude more than the median member).
The average earnings for a US doctor is around $188,000, over 3 times the US average income of $49 640.7 The average earnings for a UK doctor is £70 648, well over double the UK average salary of £27 100.8 Both US and UK doctors are in the top 5% of incomes in their countries.9
Income varies due to seniority (junior doctors earn much less than ‘fully fledged’ physicians – but progression in medicine is fairly reliable), specialty (across the OECD specialists earn more than general practitioners/family physicians)10, and location (both inter and intra-nationally).11 Variation is marked: the 90th percentile of UK doctor’s salary is £131 29812, nearing double the ‘average’ UK doctor; the average earnings for a US anaesthetist is $246,340. However, there appears less variation than other lucrative professions (e.g. finance, corporate law) likely because the medical hierarchy flattens at the top: the majority of doctors reach the ‘final’ or ‘highest’ rank (consultant/attending physician, GP principal, etc.), and so their level of seniority and compensation are on a vague par. Not so careers with a pyramid like hierarchy, with some people either being ‘stuck’ on intermediate rungs of the ladder without further progression; or those in which many have to leave to a less lucrative career due to an ‘up or out’ model.
Reasons against medical careers
Modest direct impact
Ironically for a profession in which most applicants cite humanitarian or altruistic reasons, the impact of practicing medicine – particularly in the developed world – is limited. This is for several reasons:
- A clinician can only treat the patient in front of them. Thus good clinical practice can’t ‘scale up’ in impact the same way research breakthroughs or policy changes can.
- The ‘inverse care law’ (healthcare resources – doctors included – tend to be concentrated in the areas of least need) is well demonstrated within and between countries.13 This misallocation makes clinical practice very crowded and far from neglected, and so the expected ‘returns’ have diminished substantially. To a first approximation, marginal doctors in the developed world is straining for hard-to-reach medical benefits for populations who are amongst the healthiest on the planet.14
- It is widely accepted that ‘social determinants of health’ (wealth, socio-economic status, sanitation, education, among others) are much more important than the work of the medical profession in keeping people healthy.
- Medical schools are over-subscribed, so the counter-factual of declining to apply to medicine is not there being ‘one fewer doctor’, but closer to a minor change in the aggregate supply of medical students, or an even more minor change in their expected quality. The impact of this is far smaller than there being ‘one fewer doctor’.
The health economic literature has not directly looked at the ‘impact of a doctor’ in the western world. I have performed my own research looking at international patterns of health (either life expectancy or health-adjusted life years) and physician density to extract a ‘marginal impact of an additional doctor’, both ‘raw’ and when correcting for other determinants of health that vary between countries (e.g. wealth, education).
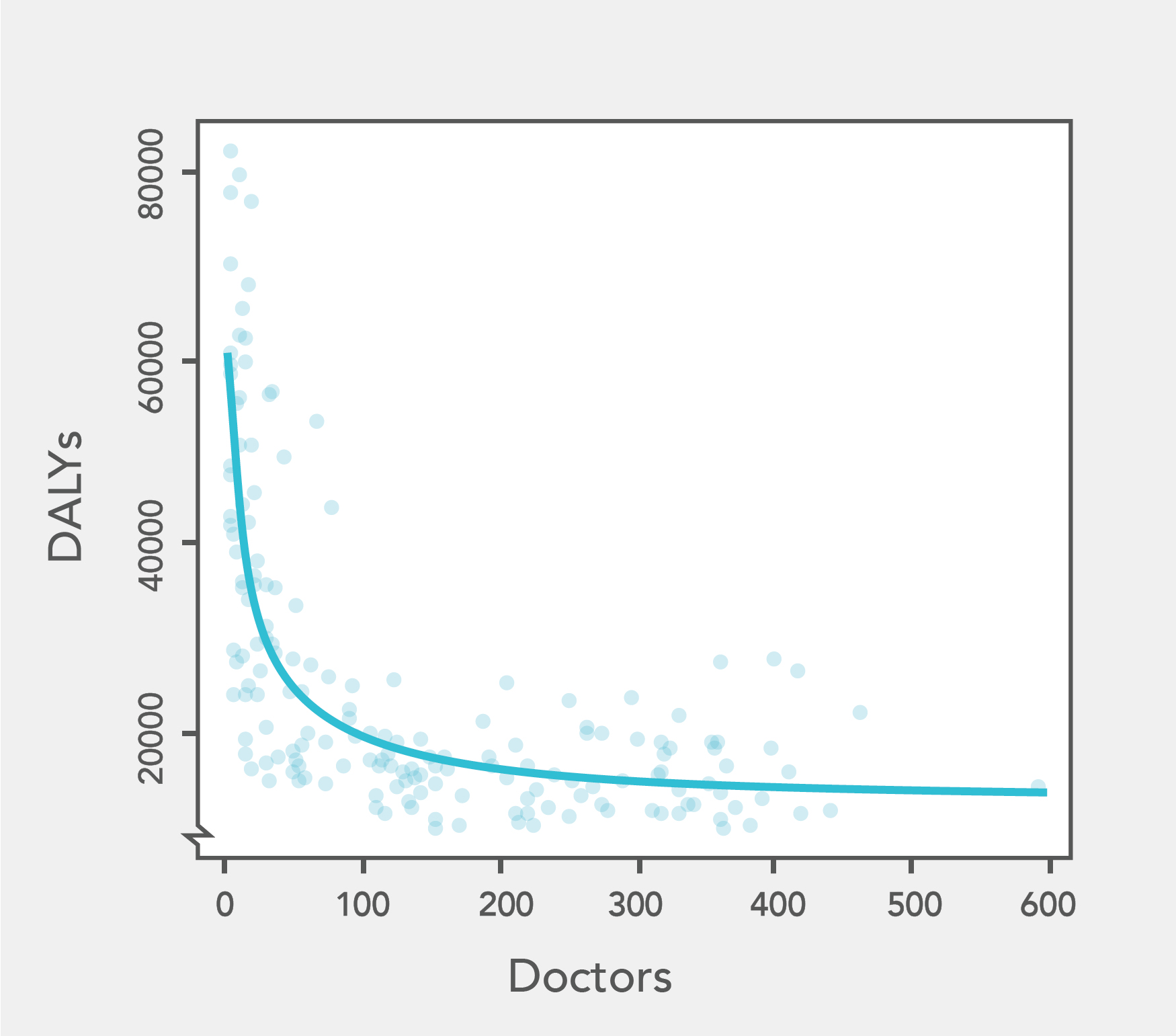
This analysis confirms the contentions above: physician density is negatively correlated with burden of disease15; the social determinants of health explain more of the variance in health outcomes than physician density16; there are steeply diminishing returns between increases in physician density and decreases in burden of disease15. Further, the ‘bottom line’ figures (which are likely optimistic) suggest an additional doctor adds four health years for every year they work. This is a lot less than can be accomplished through even modest donations to effective charities, and so suggests the ‘direct impact’ of medicine is pretty modest.17
Competition
Entry into medical school is notoriously competitive, and thus medical schools can be highly selective for academic performance. However, competition conditional on being accepted into medical school is much milder, so the likelihood of ‘making it’ as a doctor after being admitted to medical school is high.
In the US in 2014, there were 19 517 successful applicants out of a total pool of 45 266, for a ‘success rate’ of ~43% – but applicants were self-selecting. For those being admitted for M.D. degrees, the average GPA was 3.69 (A-) and the average MCAT score was 31.4, both around the 80th percentile of university graduates18 (and, in the MCAT’s case, there is significant further self-selection).
For the UK in 2014, there were 84 850 applications for 6 820 acceptances. However, each person could make four applications to medical school. Assuming they did so, this suggests approximately 21 200 applicants, and so a ‘success rate’ of 32%.19. The average UCAS tariff (total of all AS and A-level grades) for successful applicants to medical schools in the UK was 536, corresponding to slightly better than AAAA at A-level (520 points). Around 4.9% of A-level students got AAA or higher in 2012.20 This tariff is similar to some ‘elite’ undergraduate degrees in the UK: e.g History at Oxford (544), Engineering at Imperial (546), Politics at Cambridge (549); however, others are much higher, e.g. Mathematics at Cambridge (642), Economics at Oxford (598).21
Medical schools also select on aptitude tests: the UKCAT and BMAT. Although the data is patchy, the evidence is suggestive that successful applicants generally score one standard deviation or more above the mean.22
An indirect approach to assess how competitive medical schools are is to look at the IQ of medical students and doctors compared to the general population (although it should be noted that the data available is from 1940-1972). Doctors and medical students consistently average around 125-130, in the top 5% or so of the population. To benchmark, one small study puts the average IQ of Harvard undergraduates at 12823, and another put the average IQ of Cambridge academics in a similar range.24
In summary, medicine selects highly intelligent and academically able people, and the strength of competition for medical school appears approximately similar to other ‘elite’ educational achievements.
Career capital
On the face of it, a medical degree has good career capital. Completing a medical degree is a signal of intelligence, conscientiousness, and capacity for hard work, all valued by employers [(e.g.)](https://www.mckinsey.com/careers/students/tips-for-advanced-professional-degree-candidates. Doctors can wind up transitioning into prestigious careers like consulting, or finance. Closer to home, they can become involved in health policy, management of health services, or scientific research.
However, when adjusted for the significant time investment (at least 2-3 years ‘beyond’ undergraduate in undergraduate-entry systems like UK, at least 5 in graduate-only ones like the US) and monetary cost (average debt at graduation of $170 000), it looks much less promising. Although doctors can end up in (e.g.) finance or consulting, it seems that a better path to these careers would be to enter them directly after an undergraduate degree instead of after medical training. For many of these careers (e.g. finance, consulting, entrepreneurship), spending the years one would have spend in medical training in these careers instead will likely result in better career capital at the same stage.
Advocacy
Doctors are thought to be one of the most trusted professions, most prestigious, and in a study looking at perceived both warmth and competence, scored very highly on both axes. One would expect these positive perceptions by society at large confer an advocacy advantage to doctors.
However, this does not translate into significant influence. Looking at the professional backgrounds of Congresspeople and Senators and Members of Parliament reveal doctors are much less well represented than many other professions, not only law, politics, and business, but also farming, teaching, and academia. Although there are individual case studies of doctors being public figures, (e.g. Atul Gawande, Ben Goldacre and Hans Rosling), their influence is circumscribed to health. Medicine, despite its advantages, does not reliably grant a strong public platform or great opportunities to influence.25
Conclusion
Given the above, we lean against recommending medicine. Given how competitive it is, the people who have a good chance of succeeding at entering a medical degree likely also have a good chance in other highly competitive fields which have better prospects of direct impact, advocacy, or earning to give.26
We would recommend medicine to those who have a much better personal fit for it than other candidate careers, and it seems a strong ‘first step’ for those with a strong preference for making an impact through a health related field.
See this brief interview for more thoughts.
What if I’m already a doctor?
We recommend — especially for doctors early in their career — slanting your efforts more towards the promising areas within medicine (biomedical research, health policy work and public health, possibly healthcare management). Another approach, especially for later-career doctors who are in the ‘wrong’ field, is trying to maximise income for earning to give.
Check out High Impact Medicine, a group dedicated to maximising impact in medical careers for more analysis and community help.
Can clinical practice be high impact?
There is little data which can help answer the question, “Which medical specialty has the highest impact?” The best heuristic would be to try and look at where the need for medical care most greatly exceeds its supply. Within the developed world, this would suggest looking for ‘cinderella’ fields are neglected due to things like being stigmatized or poorly paid (psychiatry and mental health is a leading candidate). However, there are reasons to think – particularly in health systems like the UK – there should not be too great a discrepancy between the value of different specialties, or of working in different locations.27
There appears even greater unmet demand when one looks at international (rather than intra-national) health inequality. How good might it be, then, to work for an international agency like MSF as a doctor, or to simply emigrate and work in a country with fewer doctors? It is hard to say. One ‘back of the envelope’ approach would be to re-run the numbers in my draft paper for an extra doctor in a poorer country: on this view, the impact is around 40-50 times greater. However, the impact is still fairly modest, similar to saving the lives of four young children a year, something that could be achieved by giving a relatively small fraction of an average doctor’s salary to an effective charity.
In summary, the direct impact of clinical work is not the biggest factor in the difference doctors can make, and so is not the lever we recommend doctors push on to try and make the biggest impact.
High impact things doctors can do
There are fields within the health space (but outside clinical practice) where we think doctors can do a lot of good.
- Biomedical research. A medical degree can be valuable, especially more ‘applied’ branches of bioscience such as translational medicine. Further, medicine can be a good ‘fall back option’ if a research career fails: career prospects for doctors who did not succeed at being clinician-scientists are much rosier than scientists who get stuck in multiple post-docs.
- Public health and health policy. Similarly, people with a clinical background have a premium in public health or policy roles, which can be forum for considerable impact – and, once again, a medical career always remains a good fall-back option.
- Health service management. There is some limited data suggesting that doctors make particularly good managers of hospitals and health services. It is perhaps a less promising route to high impact than the first two, but it is plausible the impact of better management can scale up, and have a far larger scope for impact, than working ‘on the front lines’ as a clinician.
Earning to give in medicine
Medicine is a stable, high earning career, so promising for earning to give. How can you maximise your income within medicine?
It depends on circumstances, but in general we recommend:
- Targeting high-earning specialities, though note that these are also the most competitive.28
- Consider emigrating to the US or Australia.
- Don’t do locum shifts – it’s usually better in the long-term just to advance your career.
See the full reasoning.
You could also consider shifting to medical consulting or the pharmaceutical industry.
What about leaving medicine?
Although medicine compares poorly to other careers we consider, this is in large part because of the long and costly training it involves. If you have completed this training (or some part of it), this cost is already sunk, and so continuing in medicine is much more competitive than ‘starting from scratch’ in another career, especially given difficulties in returning to medicine, transaction and retraining costs, etc. Leaving may still be an option worth contemplating for those who medicine does not fit well, or who find an extremely promising opportunity elsewhere.
Notes and references
- Gallup poll.
In the United States, physicians lead all major occupational groups in overall wellbeing, followed by school teachers and business owners.↩
- From the Gallup poll.


- The raw data from the payscale survey is here. I have analysed the data to derive the average ranking and percentiles of medical jobs out of all careers surveyed. Analysis spreadsheet.
For the career satisfaction percentage, the data is not directly available, but was reported by Wallstreet 24/7.
- Physician
Job types: Internist, obstetrician, anesthesiologist
Well-being index score: 78.0
Obesity: 86.0%
Pct. with health insurance: 96.7%
Pct. satisfied with job: 95.5%↩
- Physician
- BBC report.↩
- Our own analysis of the payscale survey data. See here.↩
- Shanafelt TD et al. Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General US Population. Arch Intern Med. 2012;172(18):1377-1385..
Compared with a probability-based sample of 3442 working US adults, physicians were more likely to have symptoms of burnout (37.9% vs 27.8%) and to be dissatisfied with work-life balance (40.2% vs 23.2%) (P < .001 for both).
But c.f. [Keeton K, et al. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol. 2007 Apr;109(4):949-55.](https://web.archive.org/web/20150526135608/http://www.ncbi.nlm.nih.gov/pubmed/17400859)
This national physician survey suggests that physicians can struggle with work-life balance yet remain highly satisfied with their career. Burnout is an important predictor of career satisfaction, and control over schedule and work hours are the most important predictors of work-life balance and burnout.↩
- Mean US income from the US Census Bureau (Worked, all races, both sexes).↩
- UK data taken from the Office for National Statistics’ Annual Hours and Earnings Survey for 2013. The average salary for doctors is in table 14.7a, the average salary in the UK is in table 1.7a.↩
- For the UK, percentiles by income (albeit for taxpayers) are given by the UK government, US can be derived from US Census bureau. For men and women the $150 000+ income bracket comprises 4.04% and 1.1% of the population respectively.↩
- OECD report of physician and nursing earnings.↩
- Sumner DM, Li DP. The (Paper)Work of Medicine: Understanding International Medical Costs. J Econ Persp 2011;25(2):3-25, Table 2 on page 12. The paper also has useful analysis of health spending, particularly when looking at international differences of physician income.↩
- Annual Hours and Earnings Survey for 2013, table 14.a.↩
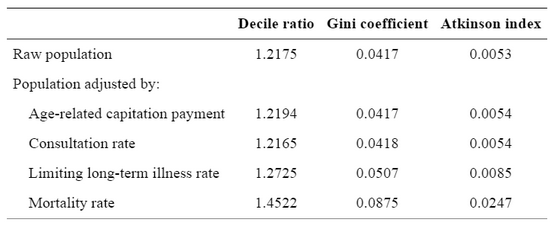
- The ‘inverse care law’ was originally coined in JT Hart in 1971. For supporting evidence, see (among many examples) Hann M, Gravelle H. The maldistribution of general practitioners in England and Wales: 1974–2003
Br J Gen Pract. 2004;54(509):894–898.Table 1 (note how the inequality measures in allocation increase when accounting for wealth, and increase further when correcting for morbidity and mortality).

Compared with patients in least deprived areas, patients in the most deprived areas had a greater number of psychological problems, more long-term illness, more multimorbidity, and more chronic health problems. Access to care generally took longer, and satisfaction with access was significantly lower in the most deprived areas. Patients in the most deprived areas had more problems to discuss (especially psychosocial), yet clinical encounter length was generally shorter. GP stress was higher and patient enablement was lower in encounters dealing with psychosocial problems in the most deprived areas. Variation in patient enablement between GPs was related to both GP empathy and severity of deprivation.
Little systematic association is found between payment quality and deprivation but, for 17 of the 33 indicators examined, delivered quality falls with increasing deprivation. Absolute differences in delivered quality are small for most simpler process measures, such as recording of smoking status or blood pressure. Greater inequalities are seen for more complex process measures such as diagnostic procedures, some intermediate outcome measures such as glycaemic control in diabetes and measures of treatment such as influenza immunisation.↩
- Several summary measures which point in this direction would be looking at the relationship between health spending and life expectancy and the (implied) diminishing returns. Another important figure would be the UK’s unofficial marginal health spend of ~£20 000 per QALY, and how is much higher that almost all developing world health interventions surveyed in DCCP 2.↩
- WHO data from 2004 (or latest available year). DALYs per 100 000 versus doctors per 100 000. Line is the best fitting hyperbola determined by non-linear least square regression. Note the negative trend (greater doctors go along with less disability burden), and the sharply diminishing returns (above ~150 doctors per 100 000, there is little incremental decline in DALYs per 100 000 with further doctors). Full explanation in my draft paper.

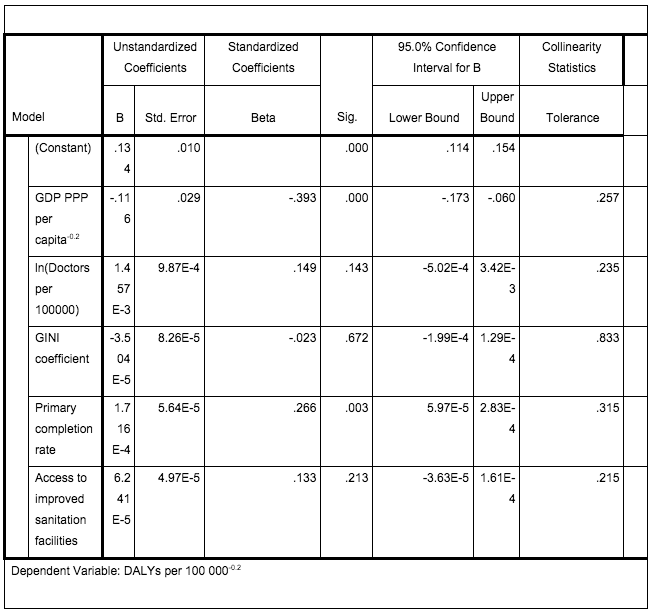
- See for example this regression analysis from Table 6 of my draft paper. (Data from WHO and World Bank).

The standardized coefficient for doctors is lower in magnitude than either GDP or a proxy for education, and thus (a fortiori) smaller than a combination of social determinants including these.↩
- See my draft paper for more recent numerical work. I am working on a more up to date analysis currently.↩
- Approximated from rank-based (‘grading on a curve’) GPAs, and thus may overestimate percentile, given other systems of allocating GPAs may be more generous. MCAT percentiles are for 2012.↩
- This should not be compared to the US acceptance rate, given the likely varying pre-selection involved.↩
- Average tariff data taken from the Guardian Good University Guide, analysis here. The data on A level proportions are from this Freedom of Information request. (N.B. There seems to be an error in how it is reported, as ‘AAA’ or better is reported twice. I am assuming that the options are ranked from AAA*, AAA, A*AA, AAA. If not convinced, a more conservative measure would be looking at AAA or above, which is ~13%).↩
- All taken from the Guardian Good University Guide.↩
- This is adduced from the score distributions of the UKCAT and BMAT, which suggest an average UKCAT score of 2520 with an SD of 280, and an average BMAT of ~5 for sections 1 and 2, and an SD of ~1. Medical schools tend to be coy about how exactly they use the UKCAT or BMAT. This collation of statements from UKCAT-using medical schools suggest many use ‘cut offs’ or have minimal scores of applicants at just below the average score, and the one school that reports averages of accepted applicants (Dundee, 2720), suggestive of selection at around the +1SD level. For the BMAT, I could only find Oxford who reports BMAT scores of successful applicants (albeit with its own reweighting), the successful applicants seem to have a mean 1SD higher than the total population.
This data should be extensively caveated. Due to the limited number of applications, students are likely to self-select: given the competitiveness of medicine, only particularly strong students are likely to apply to medicine (and hence take the BMAT or UKCAT) in the first place. Further, there will likely be self-selection within the pool of medical applicants, with stronger applicants selecting themselves to apply for especially competitive courses. Also, generally the more prestigious medical colleges (e.g. Oxford, Cambridge, Imperial, UCL) use the BMAT in preference to the UKCAT.↩
- From Carson SH, Peterson JB, Higgins DM. J Pers Soc Psychol. 2003 Sep;85(3):499-506.
The mean IQ of the sample was 128.1 points (SD 10.3), with a range of 97 to 148 points.
This may seem surprisingly low given how selective Harvard is, and that Harvard students tend to average top percentile SAT scores (which correlates strongly to IQ). This is less surprising when one considers regression to the mean: Harvard students are selected (in part) for their high SAT scores, and thus people who overperform on the SAT relative to their ‘real’ IQ will be adversely selected.↩
- Gibson J, Light P. Intelligence among University Scientists Nature 213, 441 – 443 (Paywalled). Raw data referred to in Dutton E, Lynn R. Intelligence and Religious and Political Differences Among Members of the U.S. Academic Elite. Interdis J Res Relig 2014;10:1. (page 6)
Social scientists: 121.8
Agricultural scientists: 121.6
Mathematicians, biochemists, and chemists: 130.0
Biologists: 126.1
Medicine: 127.0
Physicists: 127.7↩ - It is perhaps disheartening to note that the most significant political figure among doctors is probably Bashar Al-Assad.↩
- In very broad strokes, our view is that there is an oversupply of human capital to medicine: it attracts too many intelligent driven young people relative to its importance in the world. Hence, if we think on the margin, there should be better opportunities elsewhere for people to apply themselves.↩
- Health services should act to correct misallocations by location or workforce specialization, so that areas or specialities are not grossly under- or over-supplied. These systems are not perfect (c.f. the inverse care law), but the centralization of services in the UK gives it a chance to detect and correct these misallocations (and has a track record of making such attempts with medical staffing). It would therefore be surprising to see a ten- or hundred-fold difference in the marginal impact of (e.g.) an a cardiologist versus a neurosurgeon, or a doctor in Essex versus in Wales.↩
- Fazel S, Ebmeier KP. Specialty choice in UK junior doctors: Is psychiatry the least popular specialty for UK and international medical graduates? BMC Med Educ. 2009; 9: 77 hows good correlation between applicants per place of specialty and consultant salary.
We examined the correlation between mean income levels by consultants in each specialty and their applicants per place by UK graduates and IMGs. Estimated annual NHS consultant salaries within the specialty groups varied from £108 k (Psychiatry) to £123 k (Surgery). Expected consultant salary correlated highly with specialty popularity in UK graduates, but not in IMGs (rs = 0.85, p = 0.006 in UK graduates; rs = 0.44, p = 0.25 in IMGs).
Data from physiciansalary.com in the US shows a similarly strong correlation between USMLE1 scores and earnings of a specialty.↩