#104 – Dr Pardis Sabeti on the Sentinel system for detecting and stopping pandemics
#104 – Dr Pardis Sabeti on the Sentinel system for detecting and stopping pandemics
By Robert Wiblin and Keiran Harris · Published June 29th, 2021
On this page:
- Introduction
- 1 Highlights
- 2 Articles, books, and other media discussed in the show
- 3 Transcript
- 3.1 Rob's intro [00:00:00]
- 3.2 The interview begins [00:01:40]
- 3.3 Trying to control emerging contagious diseases [00:04:36]
- 3.4 SENTINEL [00:15:31]
- 3.5 SHERLOCK [00:25:09]
- 3.6 CARMEN [00:36:32]
- 3.7 Metagenomic sequencing [00:51:53]
- 3.8 How useful these technologies could be [01:02:35]
- 3.9 How this technology could apply to the US [01:06:41]
- 3.10 Failure modes for this technology [01:18:34]
- 3.11 Funding [01:27:06]
- 3.12 mRNA vaccines [01:31:14]
- 3.13 Other emerging technologies [01:34:45]
- 3.14 Operation Outbreak [01:41:07]
- 3.15 COVID [01:49:16]
- 3.16 Gain-of-function research [01:57:34]
- 3.17 Career advice [02:01:47]
- 3.18 Overcoming big challenges [02:10:23]
- 3.19 Rob's outro [02:20:07]
- 4 Learn more
- 5 Related episodes
Taken from an animation that depicts how Cas13 — a CRISPR-associated protein — may be adapted to detect human disease, via a diagnostic tool called SHERLOCK.
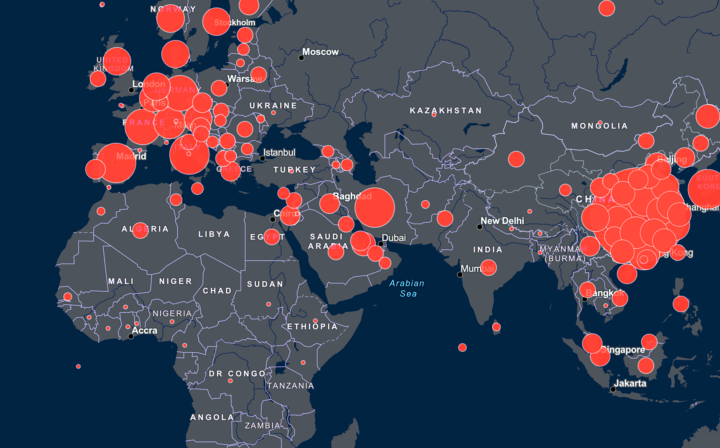
When the first person with COVID-19 went to see a doctor in Wuhan, nobody could tell that it wasn’t a familiar disease like the flu — that we were dealing with something new.
How much death and destruction could we have avoided if we’d had a hero who could? That’s what the last Assistant Secretary of Defense Andy Weber asked on the show back in March.
Today’s guest Pardis Sabeti is a professor at Harvard, fought Ebola on the ground in Africa during the 2014 outbreak, runs her own lab, co-founded a company that produces next-level testing, and is even the lead singer of a rock band. If anyone is going to be that hero in the next pandemic — it just might be her.
She is a co-author of the SENTINEL proposal, a practical system for detecting new diseases quickly, using an escalating series of three novel diagnostic techniques.
The first method, called SHERLOCK, uses CRISPR gene editing to detect familiar viruses in a simple, inexpensive filter paper test, using non-invasive samples.
Rapid diagnostic tests [are a] terrific technology, but usually it takes about six months to develop a new one because the proteins are a little more bespoke… Whereas the genome sequence, it’s just literally like a code, you just put it in and you immediately can target… You type it out and you have it going.
If SHERLOCK draws a blank, we escalate to the second step, CARMEN, an advanced version of SHERLOCK that uses microfluidics and CRISPR to simultaneously detect hundreds of viruses and viral strains. More expensive, but far more comprehensive.
Most infections all look the same — Lassa looks like Ebola, which looks like malaria, which looks like typhoid, and other things at varying stages. So you don’t want to have to know exactly what you’re looking for in a lot of cases; you want to do a broad differential that you test for.
If neither SHERLOCK nor CARMEN detects a known pathogen, it’s time to pull out the big gun: metagenomic sequencing. More expensive still, but sequencing all the DNA in a patient sample lets you identify and track every virus — known and unknown — in a sample.
Those are the kinds of technologies that we can have in the kinds of labs that we could have in every country on the planet, and even in a lot of regional centers. Then if something comes up and all the standard tests that you’ve run don’t know what it is, you can basically try to put it through.
If Pardis and her team succeeds, our future pandemic potential patient zero may:
- Go to the hospital with flu-like symptoms, and immediately be tested using SHERLOCK — which will come back negative
- Take the CARMEN test for a much broader range of illnesses — which will also come back negative
- Their sample will be sent for metagenomic sequencing, which will reveal that they’re carrying a new virus we’ll have to contend with
- At all levels, information will be recorded in a cloud-based data system that shares data in real time; the hospital will be alerted and told to quarantine the patient
- The world will be able to react weeks — or even months — faster, potentially saving millions of lives
It’s a wonderful vision, and one humanity is ready to test out. But there are all sorts of practical questions, such as:
- How do you scale these technologies, including to remote and rural areas?
- Will doctors everywhere be able to operate them?
- Who will pay for it?
- How do you maintain the public’s trust and protect against misuse of sequencing data?
- How do you avoid drowning in the data the system produces?
In this conversation Pardis and Rob address all those questions, as well as:
- Pardis’ history with trying to control emerging contagious diseases
- The potential of mRNA vaccines
- Other emerging technologies
- How to best educate people about pandemics
- The pros and cons of gain-of-function research
- Turning mistakes into exercises you can learn from
- Overcoming enormous life challenges
- Why it’s so important to work with people you can laugh with
- And much more
Get this episode by subscribing to our podcast on the world’s most pressing problems and how to solve them: type 80,000 Hours into your podcasting app. Or read the transcript below.
Producer: Keiran Harris
Audio mastering: Ben Cordell
Transcriptions: Sofia Davis-Fogel
Highlights
SENTINEL
Pardis Sabeti: We call the three tenets detect, connect, and empower. And there’s also, of course, the piece of overcoming, which is building those countermeasures. But what we were focusing SENTINEL around is just what we as a community can do. In essence, it’s building technologies to detect viruses in lots of different settings. So having these sequencing technologies that can detect and characterize a novel virus with this sort of advanced technology, on ground, in every country, hopefully in every major setting. If you see a new infection, you don’t know what it is, to be able to read out and try to uncover the origin. But then you need to be able to convert those to molecular tests that can deal with a broad differential.
Pardis Sabeti: Most people come in, they don’t know if they have COVID, or the flu, or RSV, or a host of other things. So we need to have other kinds of diagnostics that can test for a number of different viruses simultaneously in individuals that are ill, and then when there’s certain things that we know are high probability, we can turn those into point-of-care, even point-of-need, like right in the clinic, in the home, if possible. Tests that could just really pick it up closest to ground zero, right? Because you really don’t want people coming into some central place when they may have a deadly virus, because likely either they will get it or give it while they’re there.
Pardis Sabeti: So it’s to be able to have ways of detecting and diagnosing these threats wherever, and then to be able to connect that information in real time. We don’t use big data enough in medicine, often it’s just a relationship between you and the doctor and what the doctor’s recall is about what they’ve seen. Whereas you really should be able to put the symptoms into a system and pattern match, and then have the doctor overlay their knowledge on that. We don’t use that big data enough in medicine generally, but particularly in infectious disease where there’s another overlay — the network, who you are in contact with really matters — and so the other thing is making sure we can integrate the data across that piece. If there’s a lot of cases of COVID coming up in the area that you were in, there’s a higher probability the person you’re seeing has COVID. And so how do we use that information in real time and connect it?
Pardis Sabeti: And then the last piece is empower, and empower is really about empowering every actor in the system. A lot of our work has been around frontline workers, making sure they have the tools and technologies. We’re basically giving them tools so that they get real-time actionable data that also incentivizes them to give the best data. The better data in, the better information out. And so we’re trying to build these tools that work anywhere, but also through education, we’ve developed a number of programs, we’ve trained about 1,000 frontline workers so far in genomics, bioinformatics, diagnostics, other kinds of things like project management, all the things that you need to be able to run these programs, we’ve been working on building out that capacity. So that’s sort of the tenets of detect, connect, empower, and all of that is to basically get a global community working together, including every citizen, to really stave off and keep eyes on the virus and keep connected and positive with each other while we come up with these vaccines and therapies and other ways of stopping it.
SHERLOCK
Pardis Sabeti: The way CRISPR works is that it has an exquisite system of just detecting a particular sequence, and then performing a very precise cut. And we’ve been able to use that to great effect in a lot of molecular medicine. But it’s interesting from a diagnostic standpoint, there’s particular enzymes, Cas13 and more recently Cas12, that were discovered to have something called collateral effect, which means that the cut that happens has to identify a very precise sequence, so that’s where you get that sort of specificity of the cut. But then once it sees that thing, it starts cutting everything. It says, “Okay, it’s go time, we got to start cutting.”
Pardis Sabeti: And basically, Feng Zhang, who is one of the other pioneers of CRISPR is a colleague of mine, and he was working with Jim Collins, trying to use this as a diagnostic with a very a cool effect. Basically, seeing that if all that cutting is happening and these enzymes are doing that, you could then create this thing where you tie this whole system to a fluorescent readout and a quencher. So, once the thing starts cutting wildly, it’ll cut these fluorescents from the quencher and it’ll create a signal. And there’s a lot of different readouts you can use for this, including ones that can be colorimetric, essentially they can be read out on paper. So, that’s very, very powerful for getting a field deployable test. So, what’s great about the CRISPR system, in that context, and again, it’s one of the multitude of really new, exciting technologies, but why we decided to invest in that space and we like it is: It’s a molecular test. Meaning that you can basically just know a sequence and put in a sequence and make a new diagnostic immediately, that can be read out on paper.
Pardis Sabeti: So, there are these things called rapid diagnostic tests, these point-of-care tests, that have been available, but most of them are based on the protein of a virus, like the Abbott Binax where it’s an antigen capture test, it will pick the protein of the virus. Terrific technology, but usually it takes about six months to develop a new one because the proteins are a little more bespoke. They have these certain properties, you have to figure out exactly which will work and how. Whereas the genome sequence, it’s just literally like a code, you just put it in and you immediately can target, you type it out and you have it going. So, I think from that standpoint, it’s really powerful because of the fact… the PCR works in that way that it’s fast to deploy, the second the virus had it, people had PCR tests going, but this is something that’s fast to deploy, even arguably a little faster to develop than PCR, because it’s conditions are very uniform, but it can be rolled out and taken to the field and also taken to this massive multiplex that you mentioned.
Rob Wiblin: So, just to paint a picture of how useful this could be, for listeners, imagine you’re in Nigeria, in a lab out in a fairly rural area, someone comes in and it looks like they have, hypothetically, it looks like they have malaria, and you’ve got this pretty straightforward test, you’ve got the little SHERLOCK… I’m not sure what you call it, the little plastic thing, you’re going to take a blood sample, do what I think is a relatively straightforward PCR process, there’s a way of amplifying the genetic material of the pathogen in these rural areas, and then I think within hours, maybe within half an hour, you can actually say whether the person has malaria or not, which is a big step forward on having to take a sample, send it away, transport it somewhere else, and probably it’s quite a lot more expensive to do it using the normal PCR test.
Pardis Sabeti: Yeah. That is the aspiration.
CARMEN
Pardis Sabeti: CARMEN is that pairing with microfluidics, so it’s a combinatorial process. CARMEN is after Carmen Sandiego — still staying with the detective theme — but essentially it’s pairing the power of CRISPR technology with these microfluidic and miniaturization technologies to be able to do this at high scale. Most infections all look the same — Lassa looks like Ebola, which looks like malaria, which looks like typhoid, and other things at varying stages. So, you don’t want to have to know exactly what you’re looking for in a lot of cases; you want to do a broad differential that you test for. This is about having technologies that you could have anywhere in the world that you could use to test for a number of different viruses.
Pardis Sabeti: There are other groups that have developed methods like this. I’m pretty open to wherever the technology comes from. We just look to see where we can make a contribution; other groups may have technologies that end up ultimately working better. What we’re excited about with what we’re doing right now, and the need that we see, is that we haven’t seen things that can do lots of viruses on lots of samples, to be able to scale that. There are technologies that may do that, may do a differential panel, but usually still like a sample at a time or something like that. So, we were really excited that you could say, “Okay, we could take a hundred samples and run them.” I think right now in the instantiation that we just submitted to the FDA it was something that could run about one machine, about a thousand samples a day for a panel of viruses. So, that’s exciting to just be able to do that at scale.
Metagenomic sequencing
Pardis Sabeti: So metagenomic sequencing is just where the ability to read out the sequence of anything in the sample is very powerful, where in COVID amplicon-based sequencing has been really potent. It’s a little bit more directed, you have to actually have guides for the thing you’re looking for, but you can put guides for a lot of different things. So there’s just varying ways of getting more and more of a broader read of what is in the sample. And those are the kinds of technologies that we can have in the kinds of labs that we could have in every country on the planet, and even in a lot of regional centers. Then if something comes up and all the standard tests that you’ve run don’t know what it is, you can basically try to put it through.
Pardis Sabeti: It’s not always possible. The virus has to be in the sample that you’re looking for, and microbes in general are pretty stealthy. Something like Zika is causing a lot of damage, but is only there in a very small amount and for only a short period of time. And so they’re what they call “hit-and-run” microbes: they come in, do their damage, and then they disappear. So it should be noted that there’s still a lot of things that — even with all of this technology — might be missed. But that’s why we also use lots of different kinds of… There are technologies like serology-based technologies that can be better at finding the hit-and-run microbes.
Pardis Sabeti: But even when the microbe comes in, does its damage, then disappears, your immune system’s still reacting to it. And we can read out what your immune system is doing to figure out what the perpetrator was. But again, it’s all being a disease detective. And all these different clues… The way we’ve built SENTINEL, it’s not a place to test our CRISPR-based technologies. It’s a place to test and deploy and utilize the best technologies out there. And we do believe that it’s a whole series of technologies. So I think the innovation we’re trying to put forward is as much about how we do these things and how we create these hubs, where many people can come and bring their technologies and we can be honest about what’s working. We want to be able to give people feedback and say, “Hey, we tested your technology. It’s good for this. It’s not good for this. These are what you could do to advance it. This is how we’re going to use it.”
Pardis Sabeti: So trying to do the most unbiased process we can. Ultimately what motivates me when I get up in the morning is solving the problem. It’s not about the technologies I’m advancing to solve the problem, but solving the problem and being part of that process.
Failure modes for this technology
Pardis Sabeti: We’ve thought about this in varying ways. There are many different failure modes for this technology. Misuse will be a really important thing to watch for, because a lot of the technologies… We haven’t talked about the fact that things like mobile applications and Bluetooth and geolocation, all of those things are also really important and will be beneficial to a system, but have so many potential misuses. I think probably the single biggest challenge to the use of this is protecting against misuse. And at the end of the day, viruses are insidious deadly threats that weaponize your neighbor against you, and if we don’t manage that well, people can get pretty hysterical. And we’ve seen it with HIV, with COVID, with Ebola, so many different cases in which the culture becomes very toxic.
Pardis Sabeti: And so that’s one of the things that we try to build into everything we do. What’s important is this idea of making sure that the systems we put in place are ones that are thought through with regard to how they work for the communities. And that every potential misuse is considered. If you want to really stop a pandemic, you need incredible amounts of visibility. And it’s really challenging when you have all of the next generation of kids out there on TikTok and Instagram and all these places sharing all of this really personal private information with no problem, but then when it’s your location as it relates to potentially spreading COVID amongst the community, nobody wants to talk about it. There’s part of me that’s like, what’s going on here?
Pardis Sabeti: You’re literally giving away the most personal private information, but yet the thing that could actually save a life, you’re afraid to share. But at the same time, there’s a reason for that. It can be so stigmatized. And so what we’ve been doing is we’ve been piloting these types of technologies in very specific settings. When we started developing it, we were developing it for Harvard at Harvard. And the way I pitched it is the Facebook app for outbreaks, that starts within a close-knit community. A place where you can test and see how things go and get buy-in, local buy-in, and show utility to people. But Facebook can be co-opted in all sorts of bad ways, so it has to be protected and nurtured at every step.
Pardis Sabeti: And so I do think that it is about showing the use case in some environments in which there is trust, and then being able to then roll those out to other places while maintaining that level of personal-ness. I often say public health needs to be local. You can’t have somebody in Washington trying to figure out what went down in some school somewhere else. The local janitor will have more information about things, like, “Oh, well actually there’s this bathroom that everybody uses.” You actually want to empower every single person on site to be able to do this in the right way with people they trust, and in a way that builds trust.
Pardis Sabeti: There are many, many challenges, but that’s probably the one that’s foremost in my mind. How do you build these technologies? And how do you roll them out in a way that they are used well and where we remember that the virus is the threat, not each other? It is tough. And I think there’s a lot of work we have to do to build trust in society broadly in order to get there.
Articles, books, and other media discussed in the show
About Pardis Sabeti
Pardis’ work
- The Case for Altruism in Institutional Diagnostic Testing
- Emerging Disease or Diagnosis?
- Testing in a Pandemic — Improving Access, Coordination, and Prioritization
- Massively multiplexed nucleic acid detection with Cas13
- Early Detection Is Key to Combating the Spread of Coronavirus
- Profiling SARS-CoV-2 HLA-I peptidome reveals T cell epitopes from out-of-frame ORFs
- Field-deployable viral diagnostics using CRISPR-Cas13
Diagnostic techniques
- SENTINEL: Research in the time of a pandemic: SENTINEL- A proactive, early warning system to pre-empt future pandemics
- SHERLOCK: Harnessing the power of CRISPR to bring the next generation of diagnostics to the people who need them most
- CARMEN: CRISPR-based diagnostic chips perform thousands of tests simultaneously to detect viruses
- Metagenomic sequencing: Metagenomics
Books
- Contact, by Carl Sagan
- Good to Great: Why Some Companies Make the Leap and Others Don’t, by Jim Collins
Other links
Transcript
Table of Contents
- 1 Rob’s intro [00:00:00]
- 2 The interview begins [00:01:40]
- 3 Trying to control emerging contagious diseases [00:04:36]
- 4 SENTINEL [00:15:31]
- 5 SHERLOCK [00:25:09]
- 6 CARMEN [00:36:32]
- 7 Metagenomic sequencing [00:51:53]
- 8 How useful these technologies could be [01:02:35]
- 9 How this technology could apply to the US [01:06:41]
- 10 Failure modes for this technology [01:18:34]
- 11 Funding [01:27:06]
- 12 mRNA vaccines [01:31:14]
- 13 Other emerging technologies [01:34:45]
- 14 Operation Outbreak [01:41:07]
- 15 COVID [01:49:16]
- 16 Gain-of-function research [01:57:34]
- 17 Career advice [02:01:47]
- 18 Overcoming big challenges [02:10:23]
- 19 Rob’s outro [02:20:07]
Rob’s intro [00:00:00]
Hi listeners, this is the 80,000 Hours Podcast, where we have unusually in-depth conversations about the world’s most pressing problems, what you can do to solve them, and whether you told the lab you broke their centrifuge. I’m Rob Wiblin, Head of Research at 80,000 Hours.
Earlier this year I spoke with Andy Weber about a way we could use new technologies to put an end to bioweapons, pandemics and maybe contagious disease in general. We spoke about it at a high level, which makes sense since Andy is a national security person and not a biomedical scientist.
But I was left hungry to actually dig into the technical details — how do these technologies work, where would we roll them out, would people be willing to adopt them, what’s the most likely way for the plan to fail, and who might pay for it all?
Andy said I should speak to Pardis Sabeti, the rockstar scientist at Harvard who years ago co-authored a concrete implementation of Andy’s vision and has been working to get it funded, while at the same time doing cutting-edge research on ways to use CRISPR technology to improve the world.
I love interviewing natural scientists because you can actually get into the weeds with someone who works inside those weeds. These proposals really might change the world and be arriving in a hospital near you in years to come.
Pardis also turned out to be a wise person who has been through a lot in life and learned important lessons from it all.
If you enjoy this or any other episode of the 80,000 Hours Podcast, the easiest way to help us out is to leave a review of the show on Apple Podcasts, or Podchaser, or wherever else you listen to podcasts. It’s helpful because the number and quality of reviews affects how inclined people are to give the show a go when they first learn we exist.
Alright, without further ado, here’s Pardis Sabeti.
The interview begins [00:01:40]
Rob Wiblin: Today, I’m speaking with Pardis Sabeti. Pardis is a professor at the Department of Immunology and Infectious Disease and at the Harvard School of Public Health and the Center for Systems Biology, where she runs the Sabeti Lab. Among many other roles, she is an Institute Member of the Broad Institute of Harvard and MIT and a Howard Hughes Investigator. She’s previously studied at MIT as a Rhodes Scholar, at Oxford University, and at Harvard Medical School. Importantly for today’s conversation, Pardis is also one of the co-founders and a shareholder of Sherlock Biosciences, a company dedicated to improving health worldwide through accurate, fast, and affordable testing. And finally, she’s the lead singer of the rock band Thousand Days. Thanks for coming on the podcast, Pardis.
Pardis Sabeti: Hi, it’s so great to be here. Thank you so much for having me.
Rob Wiblin: I hope we’re going to get to talk about concretely how to build a diagnostic system that can detect and diagnose pandemics as soon as they appear and before they run out of control, but first off, what are you working on at the moment and why do you think it’s important?
Pardis Sabeti: I’m working on all sorts of different things that are related to pandemic preemption and response. And it’s funny because for the longest time I’ve had to try to explain why it’s important. I don’t think I need to do that anymore. It’s trying to get more concrete terms now, just because now everyone is doing what I’m doing. So it’s trying to explain the specifics of the different activities we do.
Rob Wiblin: What are the main streams of research in the Sabeti Lab? Is it mostly the diagnostic stuff that I’ve been learning about to prepare for the interview?
Pardis Sabeti: No, that’s a more nascent and smaller part of the work we do. In essence, I started my career in a field called computational biology. It’s studying the genomes of humans and other organisms on Earth to try to understand patterns that might be important in understanding our history, and impacting human health and the health of our planet. So it’s really just about using genomics and biology as mathematical information, and I just study all those patterns in nature and try to find things. And so for a long time, we were studying the human genome. It pointed us to the important impact of infectious diseases. We then started to study infectious diseases themselves and started to understand that they were much more widespread than people had thought. And it kind of led us to the field where we started studying a particular virus called Lassa that most people have never heard of and certainly only started being talked about much in the last few years, but is — like Ebola — a deadly hemorrhagic fever virus.
Pardis Sabeti: And we started working on that virus in the field. And the more we looked, the more we realized these deadly viruses were everywhere, creeping around. And that brought us to start thinking about diagnostics as a tool. We can’t study, understand, and combat these things if we can’t see them, and diagnostics let us see them. And so I think it’s a critical piece. I always follow wherever the needs are, but it’s actually not my core area of expertise.
Trying to control emerging contagious diseases [00:04:36]
Rob Wiblin: We’ll talk about the work that you’ve done on Ebola and Lassa in just one second, but first I wanted to give a little bit of a preface for listeners to help understand why we’re doing this interview today. Part of the background is that a couple of months ago, we released this episode with Andy Weber, who I think you know and have spoken to fairly regularly. And part of that was about how to put an end to pandemics and bioweapons, in his view using the diagnostics that you’re working on in combination with mRNA vaccines. And that episode was super popular. And I know it got distributed within various governments, and there’s people who are taking this idea pretty seriously and it’s getting around.
Rob Wiblin: I find that everyone seemed to think that the idea was basically worth pursuing, though I did get some responses from people who were skeptical that it would be quite as effective as Andy made out. His pitch was that it would totally put an end to bioweapons or make them useless, which is a pretty tall order. But anyway, I asked Andy which scientists I should talk to about technologies that could actually make his proposal possible and actually get it rolled out within our lifetimes, and he said you’re the person, because you’re at the cutting edge of these contagious disease diagnostics, and you were focused on this before COVID came along.
Rob Wiblin: But yeah, before we get to all of those diagnostic tools, it would be really useful to have some background on the pandemics that you’ve worked on in the past and what you contributed there. What has been your direct experience with trying to control emerging contagious diseases? I guess it’s Ebola and Lassa that are the big ones you’ve worked on?
Pardis Sabeti: Yeah. Well first I want to just say thank you for that. That’s very high praise from Andy, and I’m grateful to be here to talk about that kind of work. I think that what he’s proposing is bold and ambitious, but I think it’s something that’s in reach. If we can send a man to the moon, we can combat infectious diseases on our planet, and do so in a way that makes the world healthier — not just from staving off a potential cataclysm, but on an annual basis, reducing mortality and morbidity. So I certainly think it’s worth pursuing. It’s ambitious, but it’s possible.
Pardis Sabeti: I think the work that I’ve done in other outbreaks makes it clear. It is amazing actually, how much we’ve been flying blind for years. I mean, think of it yourself, when was the last time you were sick and it wasn’t the flu or strep and you knew what you had? I mean, it wasn’t flu, strep, or COVID, and you knew what you had? Every time we get sick, we’re just like, “Well, I hope it’s not anything too bad.” And you look around at people in the office and you wonder who gave it to you, but we don’t even ask. There’s this cultural thing where we don’t even ask, “What did you have? What worked for you?” And so it’s just amazing how little we do to educate ourselves and be responsive to outbreak spread in our communities.
Pardis Sabeti: And before this, I mean masks are now a thing, but people used to come to the office and cough on you, right? Or in schools, in class, we just sort of accept some level of this infectious disease burden. But there are tools and technologies that make it possible not to. Like I said earlier, I used to have to explain what I do and why it mattered, and now it’s what everyone does and thinks about. When you are in it, when you’re in a pandemic, all these things become very obvious to you, why you need to have better diagnostics and better responses and build all of those things and those systems. But also that they’re plausible. And if we actually invested even a fraction of what we invest in so many different programs, we would have a massive lead on how to stop infectious diseases broadly, and pandemics.
Rob Wiblin: Yeah. It’s an interesting cultural phenomenon, as you say, because we don’t really have diagnostics for anything that’s not really serious. We just have this broad category called colds. And people are just like, “I have a cold.” It could be one of hundreds or thousands of different viruses, but we’re content not knowing.
Pardis Sabeti: And also it could be a bacteria, which is very different biologically and it has to be treated in a very different way. Even in what we nutritionally give ourselves, it’s a different process. There’s a beautiful paper by Ruslan Medzhitov[inaudible 00:06:37] that explains the old adage “Starve a cold, feed a fever.” There’s a reason for that: Bacteria and viruses have different nutritional demands. There’s so much we could be doing better if we actually knew what was making us sick and what works for people when they have that specific microbe as opposed to something else.
Rob Wiblin: It reminds me of how Isaac Asimov had a bunch of stories about this superhuman race that was still recognizably human, but they’d advanced massively thousands of years in the future and they were on other planets, and they just didn’t have any diseases, any contagious diseases whatsoever. They’d managed to eliminate all bad bacteria and all viruses that they didn’t want. And that’s part of him painting a picture of a quite sterile world for them, quite a boring and very risk-averse world. But maybe we could get to the point where we could eliminate most of these viruses and bacteria in the next few hundred years with the technologies that we’re coming up with.
Pardis Sabeti: Well, I mean, the interesting thing is that we absolutely don’t want to eliminate bacteria and viruses. I think if we did that we’d probably eliminate ourselves. There are an estimated 30 trillion human cells in the human body, and there are 40 trillion bacterial cells in the human body. We are more bacteria than we are humans, and they are critical to every part of our survival. It’s not about getting rid of them. And even viruses, there are so many viruses that are helpful to us, that are integrated into our genome that are important in processes for us. So it’s not about getting rid of them. It’s about creating that healthy equilibrium and staving off pathogenic effects. Which even our own cells can have. Our own cells can act out. There’s an ecosystem and it has to just be kept in balance.
Rob Wiblin: Yeah. Let’s come back to the work that you’ve done combating the hemorrhagic fevers like Ebola and Lassa. How did you end up involved in that, and what did you try to contribute?
Pardis Sabeti: So I’ve been interested in infectious disease for a very long time. Even when I went to medical school, that was the area I was most excited about and interested in, and it might be… Actually my PhD that I did before that was studying malaria. So it’s always been an interest of mine to study this interface between humans and infectious diseases. And then I was doing my postdoc with Eric Lander at what became the Broad Institute. And I had developed an algorithm that could mine the human genome looking for footprints of ancient adaptation, basically looking for beneficial traits that arose in our genomes and rose to prevalence. And there are a number of classic ones that we know about like the sickle cell trait that rose to prevalence, because it protected from malaria, but using a way of detecting that pattern, I was able to find a lot of other things.
Pardis Sabeti: And one of the strongest signals we found in the human genome linked to a gene that’s critical for the entry of a virus called Lassa virus. I’d gone to medical school, and I’d never heard of this virus. I went back to my textbooks and it’s like noted once in a table about arenaviruses, but not described at all. It’s just not something that’s on our radar, and it sort of was stunning to me that there was this virus that the data was telling me might’ve been the most impactful virus in our human history, but yet it’s not something we think about or know about. So the signal selection we detected is in a population from Nigeria, and the virus was first described in Nigeria. So I was like, “Well, that’s interesting.”
Pardis Sabeti: And then the more I started studying the literature and connecting with my colleagues in Nigeria, the more it became clear that actually this virus is probably circulating. And no one is testing for it. I mean, no one. In none of these countries. Only in Sierra Leone had there started to be some testing on site. There were cases in England no one had tested for. No one was testing for these things. In the United States, generally there’s only one lab that tests for it, and very, very rarely, and it’s the CDC. It’s not something you’re looking for. So then of course you expect not to find it.
Pardis Sabeti: And so we worked with Christian Happi in Nigeria, partnered with the Irrua Specialist Teaching Hospital and set up the ability to do diagnostics on site. And in Germany, the Bernard Nocht Institute was starting there, so we all collaborated. We all worked together to collectively build up diagnostic capacity in this hospital. And what we found immediately was that there were a lot of cases. And in fact, the more cases we had, and the more we were able to treat those cases and give them a life-saving drug, ribavirin, the more people started coming to the hospital, because there was a reason to do so. They could get information and they could get a good outcome. And our catchment area grew and grew. And we started to see not just cases of Lassa, but all sorts of other things. Our team wrote a paper published in Science Magazine that was posed as a question: Emerging Disease or Diagnosis?.
Pardis Sabeti: These diseases that we call emerging, are they actually new or is this just the first time we’ve detected them, but they’ve actually been circulating widely for centuries? We started saying we need to actually have better diagnostics on ground, in our sites in Sierra Leone, in Nigeria. We got support from the World Bank and the NIH to build that up, and then Ebola hit. And we’d already been paying attention to Ebola at that time. In fact, the paper talks about evidence for both Lassa and Ebola to have been circulating for some time.
Pardis Sabeti: And so we were prepared, but essentially we were part of that outbreak because we’d been paying attention to that area thinking there are risks already, and the outbreak hit, it just came to us. And so our colleagues on the ground were poised and ready. They detected the first cases in those countries, and we sequenced the genomes and generated the data and made it available to others so that they could start building diagnostics and vaccines and therapies, trying to get the world to be able to move quickly to these outbreak responses.
Rob Wiblin: Amazing. What’s going on with Lassa? It seems like it’s had a large push on human evolution over the years, or we see some signals in the genome of that. It’s quite dangerous, right? But it’s circulating in these countries, and we’re not picking it up — or people aren’t noticing that it’s Lassa. This is a slightly strange picture, that it would be so obscure if it’s having such a large impact.
Pardis Sabeti: Well, yeah so there’s two parts to that. One part is that it’s amazing how much death we ignore in some of these other countries. And we group them all in as fever, and often misclassified as malaria, and we just leave it at that. So there’s some actual fatalities that we are ignoring, but there’s also — this was part of the intriguing thing — why is it that for some people it’s devastating, and for other people, they don’t get sick at all? We all know about asymptomatic infections now, but at the time it was really hard to say. That was one of the things that we described in this paper. There’s a lot of asymptomatic infections, there’s a lot of people you’re not seeing getting this at all either.
Pardis Sabeti: And if there was an ancient adaptation, that’s exactly the kind of thing you’d see. Where for some people, genetic traits that completely protect people would have emerged to prevalence, and so in some portion of the population you don’t see it at all, they either cannot be infected or not get sick from it, while other people will have devastating consequences. And what was interesting is it looks as if just a fraction of people in places like Nigeria who get Lassa get ill from it. But from what we can see, all of the non-African individuals who got Lassa had pretty devastating consequences, lots of fatality, also lots of long-term effects. And so what we suspect is that in places like West Africa, where they historically have a lot of exposure to Lassa, people have developed genetic resistance, and in other places they don’t have that.
Rob Wiblin: Yeah. That makes a lot of sense.
SENTINEL [00:15:31]
Rob Wiblin: Let’s push on and talk about the SENTINEL system (also see here), which I guess has been developed partly in response to this work, finding that there’s all of these diseases potentially circulating in places where there aren’t good diagnostic methods. I suppose the SENTINEL system seems like it could serve both purposes of understanding much better the diseases that have always been out there and then potentially treating them and containing them. And simultaneously it would also provide the infrastructure necessary to catch and contain future truly new diseases before they can spread very far. I read a proposal document you contributed to, which amusingly you published in December 2019, right before COVID-19 struck the world. Very timely. What’s the big-picture strategy of the SENTINEL system?
Pardis Sabeti: So it had its foundations in the work we were doing on Lassa fever, where when we started to see it… If we just set up diagnostics for even one thing, if we could treat just one thing, then that’s at least one thing you know you do or don’t have, right? And it’ll start bringing people into the system, it’ll start supporting the hospital, and it’s care-taking, and you can build on that. It’s a positive feedback loop where each thing that you detect brings more people in and interested in coming to the hospital, brings more cases you can investigate, potentially brings more diagnoses that you can then feed into the system and use to develop tests for new things that could be circulating. And so it’s really about building an ecosystem.
Pardis Sabeti: What’s amazing about pandemics is that they’re in that class of existential threats to humanity, right, like nuclear war and climate change, but there’s a few things that are pretty special about them. One of them is that they have been very effective, like in a very large way, year after year, century after century, and in all of history, they have been cataclysmic. And they’ve had incredible effects on both life and on the economics of human populations. And so they are things we should respond to and be prepared for. But also there’s a universality to infectious diseases: The same technologies you’re using to stop Ebola or a potential bioterrorist threat are what you need to stop that common cold going through your kid’s daycare or through the office. And so there’s a real power of just building those technologies that can be used across the pace.
Pardis Sabeti: And the other thing I would say about infectious diseases is that in other universal human things we should do, like vote or recycle, it’s hard to explain to a person why their vote matters, particularly in the United States with the electoral college, or why their recycling matters when you see businesses dumping all sorts of things into the environment. But with an infectious disease, because of the exponential spread of viruses, it is true that one person could have an outsized potential to have an impact, right? One person can launch a pandemic, and therefore one person could stop a pandemic with their actions. That’s sort of how we pitch what we’re doing with SENTINEL, is to empower every actor in the system and to build these systems that will work in times of quiet that are prepared to be leveraged in times of need.
Rob Wiblin: So what’s the machinery of the system?
Pardis Sabeti: We call the three tenets detect, connect, and empower. And there’s also, of course, the piece of overcoming, which is building those countermeasures. But what we were focusing SENTINEL around is just what we as a community can do. In essence, it’s building technologies to detect viruses in lots of different settings. So having these sequencing technologies that can detect and characterize a novel virus with this sort of advanced technology, on ground, in every country, hopefully in every major setting. If you see a new infection, you don’t know what it is, to be able to read out and try to uncover the origin. But then you need to be able to convert those to molecular tests that can deal with a broad differential.
Pardis Sabeti: Most people come in, they don’t know if they have COVID, or the flu, or RSV, or a host of other things. So we need to have other kinds of diagnostics that can test for a number of different viruses simultaneously in individuals that are ill, and then when there’s certain things that we know are high probability, we can turn those into point-of-care, even point-of-need, like right in the clinic, in the home, if possible. Tests that could just really pick it up closest to ground zero, right? Because you really don’t want people coming into some central place when they may have a deadly virus, because likely either they will get it or give it while they’re there.
Pardis Sabeti: So it’s to be able to have ways of detecting and diagnosing these threats wherever, and then to be able to connect that information in real time. We don’t use big data enough in medicine, often it’s just a relationship between you and the doctor and what the doctor’s recall is about what they’ve seen. Whereas you really should be able to put the symptoms into a system and pattern match, and then have the doctor overlay their knowledge on that. We don’t use that big data enough in medicine generally, but particularly in infectious disease where there’s another overlay — the network, who you are in contact with really matters — and so the other thing is making sure we can integrate the data across that piece. If there’s a lot of cases of COVID coming up in the area that you were in, there’s a higher probability the person you’re seeing has COVID. And so how do we use that information in real time and connect it?
Pardis Sabeti: And then the last piece is empower, and empower is really about empowering every actor in the system. A lot of our work has been around frontline workers, making sure they have the tools and technologies. We’re basically giving them tools so that they get real-time actionable data that also incentivizes them to give the best data. The better data in, the better information out. And so we’re trying to build these tools that work anywhere, but also through education, we’ve developed a number of programs, we’ve trained about 1,000 frontline workers so far in genomics, bioinformatics, diagnostics, other kinds of things like project management, all the things that you need to be able to run these programs, we’ve been working on building out that capacity. So that’s sort of the tenets of detect, connect, empower, and all of that is to basically get a global community working together, including every citizen, to really stave off and keep eyes on the virus and keep connected and positive with each other while we come up with these vaccines and therapies and other ways of stopping it.
Rob Wiblin: Okay. So there’s three components, there’s the diagnostic stage, and there’s actually three fairly newish technologies that are part of that, which we’re going to talk about in a second. Then there’s a data component, which is pulling together all those results from all of those diagnostic tests into one place where they can be properly understood and interpreted, and then there’s the response thing where you’re going to actually empower the people down on the ground to figure out how to control these contagious diseases with the knowledge that you’ve gained by bringing together all this information. Where is SENTINEL at, at the moment? Has it been funded, and is it actually getting rolled out in any countries?
Pardis Sabeti: We’ve been working on versions of this for the last probably 12 years, but it’s funny. Right before Ebola hit, we got funding from the World Bank to start something called the African Center for Excellence in Genomics of Infectious Diseases. And it was born from that emerging disease or diagnosis question of, if we set up the ability to do these kinds of testing, would you find these things? And then we got that support to start this program, and a lot of it was around education. It was around educating those individuals on the front lines to get this started, and it happened just as Ebola hit. And then as you said, we published this final document in December 2019, just as COVID hit.
Pardis Sabeti: And so we had this very interesting timing. The way I describe it is sort of with the Rolling Stones line, “you can’t always get what you want / but sometimes you get what you need.” At least we had the ability to respond in both cases at that moment, but obviously we would have loved to have preparation. So, but in the process, we basically pivoted and everybody on the planet became a COVID expert. But the thing that’s nice about it is everything changed and nothing changed. The systems we had to put in place were the systems we needed, and we already had capacity to do testing on the ground, but some of the things we were positioned to do is, we always are watching to see what viruses are circulating and whenever anything piques our attention, we make sure the hospitals on ground have the testing available, because they are the reference centers for their countries.
Pardis Sabeti: And so, yeah. I’m proud to say that we, our collaborators on ground in Sierra Leone, Senegal, and Nigeria had worked in diagnostics in their hospitals in early February 2020, basically ahead of any U.S. hospital. And so we are always moving as fast as we can. As soon as the genomes were published, we had working diagnostics and we took them out and worked with them to establish them. And then those hospitals and research centers became reference centers for their country. Christian Happi, my colleague of 20 years in different varieties and my main partner for SENTINEL and all things, he and his team sequenced the first case of, genome for SARS-CoV E in Africa, and are now a reference center for the continent.
Pardis Sabeti: And meanwhile, we were also staving off new infections, like while this is all going on, other outbreaks are happening too. And they’re doing all those kinds of detection efforts and they’re scaling up their capacity as much as possible. So they’re in it, just like everybody else on the planet, they’re in it. And they were very grateful to The Audacious Project that supported us being able to move quickly here.
SHERLOCK [00:25:09]
Rob Wiblin: So the most innovative part of this whole system is the diagnostic technologies, of which there are three really cool ones, but it seems like progress on those is the thing that’s making this possible in a way that 20 years ago, it just wouldn’t have been viable to propose a system like this. So let’s talk about those three in a bit of detail, so listeners have a good model in their heads of what might be coming down the pipeline. The three methods are SHERLOCK, then CARMEN 1, 2, and then metagenomic sequencing. What can SHERLOCK do that previously we couldn’t do?
Pardis Sabeti: I’m going to put my conflict out on the map, and there’s two conflicts I want to note. I am a co-founder of Sherlock Biosciences, but I’m also a board member of Danaher that owns Cepheid and IDT. I got into that space because I realized I want to make an impact and I want to be involved in where technology moves forward, but I do realize that that also complicates what I say here. So, please take that into account when I speak.
Pardis Sabeti: What I’d say is, actually, when you said it wasn’t possible 20 years ago, that’s not exactly true. Both the technologies have advanced, but we also have not invested in any way in infrastructure in building this. Polymerase chain reaction (PCR) is an old technology, it really advanced in the 1980s. And PCR could have done these kinds of detections.
Pardis Sabeti: We wrote an op-ed in The New England Journal Of Medicine that essentially said there are 260,000 clinical labs in the United States, and when COVID hit, and beyond, only 160 of them got FDA approval to set up a PCR test. And only another 40 or so did it without FDA approval. That’s 200 of 260,000 labs. No one moved. We rely on commercial companies to do this stuff for us. We could actually take any technology… There’s LAMP technology that I was, I’ll be honest with you, I was doing in my own kitchen. Basically, LAMP is a technology you can do with a sous cooker at home. There is a lot we could do with the technologies we aren’t doing. That said, I just want to make sure it is known that it’s not about this technology saving us, it’s about us investing in it and actually empowering people to do things.
Rob Wiblin: The latter two of these seem like they can test for lots and lots of different contagious diseases simultaneously at a much lower price than doing a PCR for every single one, one after another. It seems like it makes it maybe affordable to have really broad-scale testing for lots of different things in lots of different people in a way that previously might’ve been outside of the budget.
Pardis Sabeti: I think that’s probably a fair point. I certainly agree with you, that the time is nigh. There’s a lot of convergence happening here, but it’s multiple things. And like I said, PCR is a great technology and isothermal applications are great technologies too, that we could be using better. There are a lot of technologies that are out there that are interesting. We are particularly intrigued with CRISPR, Emmanuelle Charpentier and Jennifer A. Doudna won the Nobel Prize this year, and CRISPR has been advanced by a number of terrific folks. It’s a wonderful technology. What’s amazing about CRISPR is it’s found in nature, and its job is to detect and destroy viruses. It’s a bacteria’s immune system to phages, these viruses that infect them, and they’re just really good. It’s a very exquisite and elegant system that just looks for these viral sequences, and then once it detects them, it cuts them. And there’s a version of that where you can do it in a test tube, where if the cut happens, you can pair that to a fluorescent readout. Essentially, you have a quencher tied to a fluorescence, and when you have these cuts happen, you can disconnect the quencher from the fluorescent readout and signal it.
Rob Wiblin: So listeners can follow, there’s a molecule that would be colorful and be visible, except that the color or the fluorescence is being quenched by this other thing that it’s connected to, and you use the fact that when this Cas protein detects a particular strand, it then just starts cutting RNA all over the place, that causes it to separate and then to start being colorful and visible.
Pardis Sabeti: Sorry, I jumped through that technology, but I know your audience wants to get into the meat of it.
Rob Wiblin: I only just learned about quenching.
Pardis Sabeti: The way CRISPR works is that it has an exquisite system of just detecting a particular sequence, and then performing a very precise cut. And we’ve been able to use that to great effect in a lot of molecular medicine. But it’s interesting from a diagnostic standpoint, there’s particular enzymes, Cas13 and more recently Cas12, that were discovered to have something called collateral effect, which means that the cut that happens has to identify a very precise sequence, so that’s where you get that sort of specificity of the cut. But then once it sees that thing, it starts cutting everything. It says, “Okay, it’s go time, we got to start cutting.”
Pardis Sabeti: And basically, Feng Zhang, who is one of the other pioneers of CRISPR is a colleague of mine, and he was working with Jim Collins, trying to use this as a diagnostic with a very a cool effect. Basically, seeing that if all that cutting is happening and these enzymes are doing that, you could then create this thing where you tie this whole system to a fluorescent readout and a quencher. So, once the thing starts cutting wildly, it’ll cut these fluorescents from the quencher and it’ll create a signal. And there’s a lot of different readouts you can use for this, including ones that can be colorimetric, essentially they can be read out on paper. So, that’s very, very powerful for getting a field deployable test. So, what’s great about the CRISPR system, in that context, and again, it’s one of the multitude of really new, exciting technologies, but why we decided to invest in that space and we like it is: It’s a molecular test. Meaning that you can basically just know a sequence and put in a sequence and make a new diagnostic immediately, that can be read out on paper.
Pardis Sabeti: So, there are these things called rapid diagnostic tests, these point-of-care tests, that have been available, but most of them are based on the protein of a virus, like the Abbott Binax where it’s an antigen capture test, it will pick the protein of the virus. Terrific technology, but usually it takes about six months to develop a new one because the proteins are a little more bespoke. They have these certain properties, you have to figure out exactly which will work and how. Whereas the genome sequence, it’s just literally like a code, you just put it in and you immediately can target, you type it out and you have it going. So, I think from that standpoint, it’s really powerful because of the fact… the PCR works in that way that it’s fast to deploy, the second the virus had it, people had PCR tests going, but this is something that’s fast to deploy, even arguably a little faster to develop than PCR, because it’s conditions are very uniform, but it can be rolled out and taken to the field and also taken to this massive multiplex that you mentioned.
Rob Wiblin: For those who are familiar with all of the COVID diagnostics, it feels like a bit of a merger of a PCR — which can detect very small quantities of a pathogen, because you’re going to use a polymerase chain reaction to increase the amount of DNA and RNA, many, many fold — with the lateral flow test, where you can just do it at home or do it in the doctor’s lab without having to send a sample away for testing somewhere else, which slows things down and is quite expensive. Is that the main advantage that it has over the PCR testing?
Pardis Sabeti: Yeah. Those are key advantages, the fact that you can do it in a lot of different settings, and it has an endpoint readout, the color is its own readout that can be read out in these various ways very easily. So, from that standpoint, we do like that technology. And again, PCR is perfect and is a workhorse. There’s a lot of reasons or certain places where that might be the better technology, but we definitely think there’s some really interesting use cases where the CRISPR can have a big advantage.
Rob Wiblin: How much does it cost to test someone with one of these SHERLOCK tests? For reference, it looks a bit like a lateral flow test, it’s a little thing, you put a sample in, and then it goes up.
Pardis Sabeti: To be honest, that number keeps jumping around. It’s one of those things where we’re excited about it, because it could be something where you could get the reagents and all the supplies to cost just pennies on the dollar, or a dollar for tests, or maybe even less. I’m learning a lot about the manufacturing process and also the IP issues. One of the things that we’re dedicated to is making sure that in developing world countries, none of these IP issues exist. But there’s all sorts of challenges to manufacturing and getting things out. I don’t know if I could give you the exact number, we’re just trying to make it as small as possible.
Pardis Sabeti: One of the technologies that we developed called CARMEN, we’re really excited about because it allows you to use miniaturization. I’m working with Paul Blainey’s lab doing microfluidics in our first instantiation. We’re able to show you could run 64,000 assays at the same time to be able to get about 5,000 different reads, and that allows you to do lots of samples for lots of viruses simultaneously. One of the coolest things about that is that it actually reduces the cost. We really are able to miniaturize this full process and reduce the reagent cost per test by 300 fold. So, I think we can get to the point where we can make it very affordable to, like you said, test multiple different viruses at the same time. And that would be really powerful.
Rob Wiblin: So, just to paint a picture of how useful this could be, for listeners, imagine you’re in Nigeria, in a lab out in a fairly rural area, someone comes in and it looks like they have, hypothetically, it looks like they have malaria, and you’ve got this pretty straightforward test, you’ve got the little SHERLOCK… I’m not sure what you call it, the little plastic thing, you’re going to take a blood sample, do what I think is a relatively straightforward PCR process, there’s a way of amplifying the genetic material of the pathogen in these rural areas, and then I think within hours, maybe within half an hour, you can actually say whether the person has malaria or not, which is a big step forward on having to take a sample, send it away, transport it somewhere else, and probably it’s quite a lot more expensive to do it using the normal PCR test.
Pardis Sabeti: Yeah. That is the aspiration. One of the other pieces we did some early work on, and other people are also working on, something we published during the Zika epidemic, was this protocol called HUDSON that is tied to our SHERLOCK work, but HUDSON uses heat and chemicals to unlock the viral genome. So, the thing is, the PCR that we talk about in the readout, there’s all this upstream work you have to do about taking the sample, extracting the microbial genomic material, and using that to get a readout. But every step of that, you can decrease. You can make the time shorter and the cost cheaper.
Pardis Sabeti: And so, Cameron Myhrvold and Catherine Freije, and my group who led this work were able to show that they could take this… We were studying Zika and Dengue at the time and they showed that you could take samples that are non-invasive, like saliva or urine, and you could use heat and chemicals to extract this and do this whole process. So, what was really cool about that is there was no blood draw. These viruses are in a lot of different compartments of our body, so we could do something that’s totally non-invasive, and then not need to use any equipment for extraction, or equipment for these other pieces. So that is the hope, that you can really get this to the point where it can be read out. We even have some work that we’ve been doing at room temperature where this works, so all of that is really exciting and fascinating, that it could be something that could be totally end-to-end deployable.
CARMEN [00:36:32]
Rob Wiblin: That’s pretty cool. But I think the next thing is even cooler. As I understand it from the 2019 plan, so someone comes in and you think they have malaria and you test them for malaria, but if they don’t come back positive for malaria, but you know they’re sick, then you want to escalate to a second layer of diagnosis, which you call CARMEN. What can CARMEN do that was challenging before, and is additional beyond what SHERLOCK does?
Pardis Sabeti: CARMEN is that pairing with microfluidics, so it’s a combinatorial process. CARMEN is after Carmen Sandiego — still staying with the detective theme — but essentially it’s pairing the power of CRISPR technology with these microfluidic and miniaturization technologies to be able to do this at high scale. Most infections all look the same — Lassa looks like Ebola, which looks like malaria, which looks like typhoid, and other things at varying stages. So, you don’t want to have to know exactly what you’re looking for in a lot of cases; you want to do a broad differential that you test for. This is about having technologies that you could have anywhere in the world that you could use to test for a number of different viruses.
Pardis Sabeti: There are other groups that have developed methods like this. I’m pretty open to wherever the technology comes from. We just look to see where we can make a contribution; other groups may have technologies that end up ultimately working better. What we’re excited about with what we’re doing right now, and the need that we see, is that we haven’t seen things that can do lots of viruses on lots of samples, to be able to scale that. There are technologies that may do that, may do a differential panel, but usually still like a sample at a time or something like that. So, we were really excited that you could say, “Okay, we could take a hundred samples and run them.” I think right now in the instantiation that we just submitted to the FDA it was something that could run about one machine, about a thousand samples a day for a panel of viruses. So, that’s exciting to just be able to do that at scale.
Rob Wiblin: Just to put it in the most basic language, the idea of CARMEN is that you take a sample from someone, a saliva sample say, and then you test it for 200 different viruses simultaneously with the same test. It’s miniaturized, and each virus corresponds to a different square on this diagnostic block. So, it’s like running 200 lateral flow tests simultaneously on the same piece of paper. Is that the idea?
Pardis Sabeti: It’s even cooler. That first version that we had, these droplets combine and they’re color-coded and you know based on the color. They have an enormous amount of these color codes, so they know what sample and what target is in there because of it. That version was phenomenal. And then more recently, we’ve been partnering with Fluidigm using their really great technology in microfluidics to have it be these tiny little geographically separated spots on the array. So it’s very, very cool and very powerful. Like you said, it’s just completely miniaturized, so you can do a lot.
Rob Wiblin: How technically challenging is it to use? Both at the moment and also where might it be in ten years’ time?
Pardis Sabeti: We were supported by DARPA for the first project, and I think actually, our program officer Renee Wegrzyn, who is such a supporter of us. She was quoted in a piece in Nature on our work, saying “That work broke open the door in terms of what is possible.” She actually came when we put CARMEN together. We published our paper in Nature. The paper came out in early 2020, but we’d had that data for a long time, and she had come to see what it looked like. What was this thing that could do 5,000 tests simultaneously? I think she points to the time when she came into the lab and saw that it was just like the size of your hand as the moment where she was like, “Oh, this is possible.” It’s pretty impressive how modest the footprint is for what you need to do something really, really powerful. The thing about all these CRISPR technologies and other types of cutting-edge new technologies is they’re relatively nascent, and there’s a long process between getting something from the lab out into production mode, to the manufacturer.
Pardis Sabeti: That version of it was not really ready to get out into the world in a big fashion, but Fluidigm has a device that works very, very well with what we were doing, so we were able to convert that technology and that biochemistry over to their platform, and that is ready. We submitted to the FDA and are in conversations with them about where we are in the emergency use authorization pipeline, but it’s technology that is working and can work in a clinical lab, and that has been running at the clinical lab at Mass General Hospital. So, what’s remarkable about it is that we went from publishing the technology in first instantiation in 2020 to being able to submit to the FDA in 2021.
Rob Wiblin: Now it’s in use, a year later.
Pardis Sabeti: Yeah, still looking to get that FDA authorization, but it’s working in that lab and it’s generating beautiful data, really beautiful data.
Rob Wiblin: Do SHERLOCK or CARMEN require complex or expensive machinery, or chemicals that might run out during a pandemic, or might be difficult to deliver to remote areas? Are there ongoing inputs that people need?
Pardis Sabeti: There are ongoing inputs that people need for those types of technologies, but that’s similar to any…you need those reagents constantly in PCR, or anything like that. One of the breakthroughs we’ve made — and I think others have made — is being able to lyophilize these things to dry them down so that they can be sent over. We’ve had these technologies working in Sierra Leone and Nigeria, in our labs there. There is a set of reagents that you need, but all of these things need that.
Pardis Sabeti: Often we talk about the fact that there shouldn’t be any single “winning” technology, because a lot of times you’ll find out one region will run out of something and then you want to switch. So clinical labs often have a lot of redundancy, where they have multiple tests or something, because they never want to be stuck when reagents are held up or something. So, yes, there are reagents and supplies, but part of it being deployable is the fact that they can be sent over and basically dried down so that they can work after long periods of being on a shelf.
Rob Wiblin: So, with being able to test someone who comes in for hundreds of different viruses and bacteria all simultaneously from one sample, how does being able to tell whether they have a known virus help us tackle unknown viruses or unknown pathogens as well?
Pardis Sabeti: Well, in a couple of ways. It’s that you’re basically a disease detective. Any piece of information, positive or negative, helps you either rule in or rule out. If you have tests for known viruses, you can take these individuals and you can quickly identify who is known and who needs to continue to be investigated. So, from that standpoint, it’s helpful. But also that positive loop that you have… The more you can give people information, the more there’s an incentive to come in, because you can at least say, “Hey, I don’t have COVID.” Or, “I don’t have the flu.” Or, “I don’t have Ebola.” There’s something remarkable about getting a diagnosis, regardless of whether it’s positive or negative. But of course the better we get at characterizing these novel things and turning those into tests that could be used on the ground for people, the better. So, it’s a slow process of getting that information, but you have to create a process by which you… It’s a turn wheel. The more information that comes into it, the faster it moves, and the more you can keep improving a process and getting better at it.
Rob Wiblin: So, CARMEN, it seems to me, it could potentially be completely revolutionary. I’m amazed that people aren’t talking about it more, because we’re just not that far away from me being able to go into the doctor, I feel sick, they take a saliva sample, the machine works, and then they test me for hundreds of different things simultaneously, and they’re going to be able to diagnose me in a way that currently is just unviable. Currently nobody even really bothers until the condition gets to be really bad. Is it just that people aren’t talking about it because it’s so new?
Pardis Sabeti: I don’t know. It’s a great question. I’d like you to go talk to some folks for me, that’d be great, because I don’t know… It’s so interesting, because for the longest time, I’ve found that it’s been really hard to get people to care about pandemics. It’s been impossible. And finally I’m like, “Oh good. Now everybody gets the problem. Everyone gets this is an issue.” But everyone only thinks about COVID and nothing else. So, now this is a new problem, where they’re like, “We just need to be able to test for COVID.” I’m like, “No. You need to test for other things. That’s the whole point.”
Rob Wiblin: “…have you learned nothing?”
Pardis Sabeti: I don’t know what it takes for people to realize. There’s this sense of like, “Do we really need this?” And I say you do. People don’t know what it’s like to live in a world where you just know exactly what you have. Another thing I hear people say is like, “What difference does it make if you know what you have?” And I’m like, “You can’t answer that question, because you’ve never known.” Once you have enough people that have, say, RSV, and you realize that e.g. avocado — or whatever — is what you need when you have RSV… You can’t actually start treating the thing until you know the thing.
Pardis Sabeti: Different viruses and different bacteria have different pathophysiological processes. We’d get much better at answering all of those downstream questions if we had the upstream information of what people have. And we see this with cancer, where people got really into now understanding: What exact cancer? As it turns out, it matters. Exact cancers will give you exact therapies. And we’re not at that point where we know the exact infection, even though it’s so easy. Cancer is very hard to diagnose. You have to sequence the whole genome and start looking for patterns… Infectious diseases are not. If there is an enterovirus in you and you are sick…these are easy.
Pardis Sabeti: When it comes to precision medicine, it’s actually one of the easiest things to hit and be successful at. I don’t know why it’s not incentivized and why it’s not prioritized. It will take another several trillion dollars for us to think maybe we should be ahead of the other ones, I don’t know. I’d love for people to think about this, but yeah, we’re excited about the technology, we believe in it, and we think that this and other kinds of technology that allow you to test for lots of things simultaneously is what is needed and what will change the world. But it seems as if it’s not on people’s radar enough right now.
Rob Wiblin: So just to reiterate and dwell on this for a minute, I guess I’m especially interested in all of this stuff because it can prevent the worst-case pandemic scenarios, the next Black Death that actually kills half of humanity and it’s an absolute colossal disaster that takes civilization off the rails. That looms large in my mind. But it would also be amazing if at the same time we could get rid of all of these contagious diseases that we’ve just learned to accept, because we think that it’s impossible to get rid of the flu, or it’s not possible to get rid of all of these colds and other gut diseases that people get. So that’s one thing that would be useful even in first world countries, is getting rid of these diseases that are irritating and affect people all the time, but aren’t the end of the world.
Rob Wiblin: But then, of course, there’s many countries in the world where contagious diseases are doing much more damage. They’ve got a much larger share of the health burden. And we desperately need these diagnostic tools in order to get rid of diseases that are killing very large numbers of people. In the past we were just like, “Ah, people are sick.” There was this broad category of people who are ill, and we think it’s the spirit or we think it’s this or that, but they couldn’t diagnose people. And so it’s just a complete dead end to try to figure out what treatments you would do, because it turns out that you need different treatments for different conditions. And to some extent we’re in this state with mental health now. We’re like, “Oh, this person has depression,” but in practice, depression is probably 20 different things.
Rob Wiblin: Or maybe it’s a spectrum with lots of different pieces where different approaches would be really useful, different SSRIs might help with some conditions, but not others. And until we can break it down and figure out actually what you have and what’s going to work in that case, we can’t really make a whole lot of progress on fixing that problem. And likewise, improving these diagnostics in this case, it’s just going to make it possible to actually treat people for diseases that presently we just have to live with. Anyway, that’s my rant. Just reiterating your point.
Pardis Sabeti: Yes. I love it. I love it. Yes. Thank you. Thank you for that rant. It was very satisfying for me.
Rob Wiblin: At the start of last year, when I was talking to pandemic-focused people, they all said, “The real worry is, people are going to get really interested in this. They’re going to spend a whole lot of money and they’re going to spend it all on extremely specific COVID stuff that does absolutely nothing when the next thing comes along.” Now, it hasn’t actually been as bad as that, because we’ve made progress on mRNA vaccines, which are this fantastic platform that can be applied to lots of different stuff. And I guess we’re coming along with these diagnostic platforms that might be able to help find the next pandemic really early. It is true that we spent most of the money on the COVID-19 specific stuff rather than the platforms, but by accident, we have actually almost gotten there. We’ve gotten so close to where we need to be.
Pardis Sabeti: I think that’s a great thing though, because viruses are all very similar, and the technologies that you need to fight one… It’s not completely plug and play, but there’s a lot of overlap. So from that standpoint, that’s the part that’s been really good. They’re still myopically focused on COVID-19, but at the same time that still does a lot. And so that part I’m excited about. But I do think it is that moment where we should branch out a little bit and look more broadly, because these threats are looming. And one of the things I say is, “I need people to stop calling it a once-in-a-century event.” You can’t just say that, just be like, “Oh, but it’s a once-in-a-century event, so we’re done.” That’s not how it works. Ultimately, this may be the new norm.
Pardis Sabeti: And obviously there’s a lot of controversy right now about the lab leak and all of those kinds of things. And I think the jury is very much out. I’m staying out of that one, because I don’t know enough to say something meaningful about it. But I think the main thing I say about that is I think it’s very dangerous when we start fighting amongst ourselves. Whatever happened, or however these things might get out, the fact of the matter is they can get out in the future. Whether it’s a natural or accidental release — or heaven forbid, a purposeful release by a bad actor — we’re in a new world where all of these things are possible, and we have to get our act together as a community. We have to build systems of trust to really support each other in this, because there’s a lot to do and it’s a very precarious road ahead.
Pardis Sabeti: I always go back to that book Contact by Carl Sagan, when the protagonist is asked if she had an opportunity to meet an advanced race that built a technology to get to Earth, what was the question she’d ask. And she said it would be, “How did you survive your technical adolescence without destroying yourself?” We are in a technical adolescence where we have all sorts of technologies that are more powerful than ever before, and God knows what we’ll do with it in the years ahead. And I think that we have to build systems where we advance technologies, but we have to also do it in a way of trust and respect. Viruses thrive when we fight amongst ourselves. So there’s a lot of dangers there.
Metagenomic sequencing [00:51:53]
Rob Wiblin: So I said there were three different, really cool diagnostic technologies that were part of the SENTINEL system, first was SHERLOCK, then there was CARMEN. And the third one is metagenomic sequencing. So if you do CARMEN, you tested for hundreds of viruses or hundreds of pathogens and none of them come back positive, now you’re like, “This is a bit more of a mystery. Maybe it’s something new. Maybe it’s something really obscure. We actually just want to send off the sample and get the full thing sequenced.” So you just sequence all of the DNA, all of the RNA that’s in there. And then hopefully you’ll be able to use that data to figure out what’s going on. Is that the long and the short of it?
Pardis Sabeti: Yeah, that’s right. So metagenomic sequencing is just where the ability to read out the sequence of anything in the sample is very powerful, where in COVID amplicon-based sequencing has been really potent. It’s a little bit more directed, you have to actually have guides for the thing you’re looking for, but you can put guides for a lot of different things. So there’s just varying ways of getting more and more of a broader read of what is in the sample. And those are the kinds of technologies that we can have in the kinds of labs that we could have in every country on the planet, and even in a lot of regional centers. Then if something comes up and all the standard tests that you’ve run don’t know what it is, you can basically try to put it through.
Pardis Sabeti: It’s not always possible. The virus has to be in the sample that you’re looking for, and microbes in general are pretty stealthy. Something like Zika is causing a lot of damage, but is only there in a very small amount and for only a short period of time. And so they’re what they call “hit-and-run” microbes: they come in, do their damage, and then they disappear. So it should be noted that there’s still a lot of things that — even with all of this technology — might be missed. But that’s why we also use lots of different kinds of… There are technologies like serology-based technologies that can be better at finding the hit-and-run microbes.
Pardis Sabeti: But even when the microbe comes in, does its damage, then disappears, your immune system’s still reacting to it. And we can read out what your immune system is doing to figure out what the perpetrator was. But again, it’s all being a disease detective. And all these different clues… The way we’ve built SENTINEL, it’s not a place to test our CRISPR-based technologies. It’s a place to test and deploy and utilize the best technologies out there. And we do believe that it’s a whole series of technologies. So I think the innovation we’re trying to put forward is as much about how we do these things and how we create these hubs, where many people can come and bring their technologies and we can be honest about what’s working. We want to be able to give people feedback and say, “Hey, we tested your technology. It’s good for this. It’s not good for this. These are what you could do to advance it. This is how we’re going to use it.”
Pardis Sabeti: So trying to do the most unbiased process we can. Ultimately what motivates me when I get up in the morning is solving the problem. It’s not about the technologies I’m advancing to solve the problem, but solving the problem and being part of that process.
Rob Wiblin: Andy Weber had this vision for having a genomic sequencer in every doctor’s office that’s used as a matter of course. In a way that might be a lot simpler, because it’s just one thing, you connect it to the wifi so you collect the data from the sequencer in some central repository. Presumably that’s a lot more expensive, and that’s why you’ve designed it with this three-stage system where you want to start with the easiest, fastest, cheapest thing first, and then only escalate to the sequencing when it’s really necessary to get a diagnosis?
Pardis Sabeti: So certainly there’s a future where we all have sequencers in our home. And again, you don’t ever want to come to a doctor’s office, a central location, to find out what you have, when you can avoid it. You’re sick, you don’t want to get out of bed. There is a world in which you actually really want it at your home, but we’re not quite at that world yet. And so, yeah, it’s interesting because we are building technologies that we hope will one day be obsolete, but it’s solving the problem now, advancing the field where it needs to go, and then seeing. But I have a feeling that for some time there’ll be a utility of these different tiers of… You don’t need to really read out everything in your genome every time you get sick. This is a process we did for encephalitis. Meningitis and encephalitis are inflammation of different parts of your brain’s central nervous system. And they cause a lot of damage and they can lead to coma and death. And what’s unfortunate is so many cases of encephalitis go undiagnosed.
Pardis Sabeti: We and others, like Joe DeRisi and Mike Wilson, have done studies where we’ve studied people with encephalitis and sequenced everything in there, and you can sequence it to pieces and you still often don’t find anything. So a lot of times it’s auto-inflammatory, or it’s one of these hit-and-runs. And then when you do find something, it’s often about eight things. So why would you necessarily sequence every single time? It might not make the most sense. So at least for now, for all practical purposes, it’s actually more sensible if you try to find the thing you’re looking for, instead of getting everything coming up just to find something. So for things like encephalitis, we think that kind of panel test is probably better for some period of time.
Rob Wiblin: Yeah. Speaking of that, when I was pitching the approach of, let’s just sequence everyone who’s sick all the time, and we’ll use that to pick up new pandemics, a lot of people had this skeptical reaction where they’re like, “You’re taking all of these massive genomic sequences of everyone’s spit samples every time they’re sick, aren’t you just going to end up with this massive pile of extremely hard to interpret data that’s full of harmless viruses that are in people, harmless bacteria that are in people all the time, their own genetics and other fragments that happened to be there? Wouldn’t it be extremely hard to take all of that and actually identify that a new pathogen is in there and that a new pandemic is starting?” Are they right to be worried about that?
Pardis Sabeti: They’re right to say that we’ve got data problems and the data’s expensive and mining through all of that stuff is part of it. And one of the things we like about CARMEN is it’s so sensitive and specific. The readout is lovely. It’s like not, not, not, not…there it is. And often it’s pretty cool because you don’t usually find just the one virus in there, you’ll find the one virus plus an anellovirus, because anelloviruses are in a lot of blood samples. So it’s even better. You find the thing and then something else that’s usually in samples and then not anything else. So it’s a very satisfying output. If you could get all of the data and the data is meaningful, and we have an understanding of how to interpret it, it’s great to get it. And we always do whenever we develop a new test.
Pardis Sabeti: Like for CARMEN, every sample that we tested with CARMEN, we also metagenomic sequenced to say, what else was in there? What could we have seen but missed? And generally what we found is, yeah there was a whole lot of noise and other random junk. And then one of the powers is it found what it was supposed to find and it didn’t find other things. So yes, there will definitely be a lot of data. To me, it’s more about what solves the problem and does the best thing. And I think a lot of times this technology can be even more sensitive when you just know what you’re looking for.
Rob Wiblin: Yeah, I didn’t interrogate Andy on this too much, because he’s not a genetic scientist but I guess my thinking was presumably what happens is if we had a whole lot of these samples coming in from doctor’s offices, we’ll train the computer to just recognize like, “This is their DNA, this is a viral strand that’s in almost everyone, I’ve seen this a million times before, this is just a bacteria that’s normally in the mouth…” And just to throw away all of that stuff that you’re used to seeing in these samples that you’ve seen many, many times before and that you can pinpoint what they are. And then you’re just left with probably a much smaller set of stuff that you haven’t seen before, and then maybe you could also train the system to try to identify, “Does this look like a pathogen? Does this look like a virus of concern that we’ve seen somewhere else, or could it be a new strain of something?” So you just have to do a lot of filtering and narrowing down, but with enough data science, with enough ML, perhaps, this is a solvable problem in the long term?
Pardis Sabeti: Definitely, yeah. And that’s the kind of thing where the more you get those systems in place… We don’t have enough data to answer these questions now. A lot of times people are like, “Oh, can you predict a pathogenic virus?” I’m like, “No, because we don’t know what a pathogenic virus looks like.” For the most part, when we see the sequence, we don’t know what it means. We’re at a pretty rudimentary stage of understanding what these viruses are doing in the body and how their genomes are working. My group just published a paper, Shira Weingarten-Gabbay, a terrific postdoc in my lab just led work published last week in Cell that essentially was really studying, what is the virus presenting to the immune system?
Pardis Sabeti: Other scientists have been finding that there are these other elements of the genome, we call them non-canonical reading frames, or non-canon open reading frames, things that are off the beaten path. And in the paper Shira and the team show that those were actually presenting to the immune system too. And in fact, they’re stimulating a T cell response that in some cases is stronger than the strongest T cell response to the proteins we know. So what’s all going on there? Viruses are tiny, but they’re really compact and they have a lot of stuff they’re programming. To be able to have this tiny little genome come in and do all this damage…they’re acting as master regulators. They’re turning on and off things, they’re switching things, and until we understand all of the pieces of that, we won’t know what is bad and what is not.
Pardis Sabeti: So the more we know, the more we investigate… I describe where infectious disease is at as where modern medicine was at before the human genome was sequenced. When you’re looking at one part of the genome and trying to say something, you’re shooting in the dark. You’re trying to put a puzzle together with a couple of pieces. You don’t know what’s going on, but once we actually start, every person comes in, you know what they have, you see the genome… When you start connecting that with symptoms and cases and all of that stuff, then we can start, the whole thing will fill out. But we’re just in a place where we’re so in the dark that to say anything about what’s a pathogenic virus is almost impossible because we don’t know enough about what a non-pathogenic virus looks like.
Pardis Sabeti: That’s one of the reasons why we also want to look in nature. We don’t only want to look in clinical cases, we want to look at the same virus out in nature and say, “Why did this one jump to humans? And why did this one make people sick? And this one didn’t?” So that’s why there are all these projects of the One Health concept of making sure we understand everything in the entire ecosystem.
How useful these technologies could be [01:02:35]
Rob Wiblin: Okay. So to wrap up this section on these three diagnostic technologies — SHERLOCK, CARMEN, and the genetic sequencing — and to paint a picture of how useful they could be, I guess we could imagine if this system had been in place in Wuhan in 2019, then potentially when the first person comes into a hospital or a GP’s office who has COVID-19, which might’ve been as early as November 2019 or possibly even earlier, they would have come in, they would have taken the SHERLOCK test right away for whatever it must look like, like the flu. It comes back negative, they would have taken the CARMEN one for a much broader range of respiratory illnesses, it comes back negative. So then they’re like, “This is worrying.” And they send it off for genetic sequencing the same day.
Rob Wiblin: Maybe the next day it comes back and the system sets off a red alarm that there’s a new virus sample in here. It looks like SARS-CoV-1, so it looks extremely similar to a well-known pathogenic virus. And then maybe weeks, potentially months before we really got a full on response, things could have been thrown into high gear in order to contain this new possible pandemic. Is that the right picture for people to have in their minds?
Pardis Sabeti: Yeah, that’s right. So it could have happened even faster than it did happen. In the case of that, it still was one of the fastest turnarounds we’ve ever had to a new viral threat emerging and sequencing. And that part of it was because there was a lab there, a center of excellence that could pick up something like that. And again, in those conspiracy theories about, did it leak from the lab? How coincidental was it that a lab that was expert in doing this work is where it happened? I’d say, the funny thing is basically the whole concept of emerging disease or emerging diagnosis is you pick it up where you’re looking for it. So frankly, it could not have been in Wuhan where this thing originated. It’s just discovered where there is expertise.
Pardis Sabeti: The reason why we have so many U.K. variants is not because the U.K. has more variants, it’s because the U.K. has a really robust testing program. So from that standpoint, it’s very possible that what was once called the Wuhan virus did not come from Wuhan. It just was detected in Wuhan, because that’s where they had the expertise to do so. So from that standpoint, I think that they’re pretty on top of it.
Pardis Sabeti: I published an article in February 2020 for Time Magazine, where they asked me to write about what was going on here. And you always look back at what you wrote and you’re like, “Does it stand the test of time?” And I think it does. It basically said, “Hey, we’re actually in a really good position. They caught this thing early. The information is there, but we have to move and we have to get diagnostics in every part of the country now.” I got a lot of pushback because at the time people hated talking about viruses mutating. Even though I had published several papers about mutations in the Ebola genome. So I pushed hard and I kept it in there and I said, “But this virus can mutate, and we never know where it’s going to go and we have to move quickly.”
Pardis Sabeti: So I feel comfortable that that did stand the test of time, where ultimately, we were ahead of the game, we had gotten ourselves in a good competitive position. And one of the other things I said there was like, “It’s a respiratory virus, so it moves quickly. So we have to move as quickly. And we have to make sure the virus doesn’t get anywhere where it can mutate.” And I think part one succeeded and part two and three did not. We didn’t move quickly. We had that information, but yet the U.S. did not have testing available until March in most states, which is just way too long with a respiratory virus.
Rob Wiblin: I think even in March there was extremely limited testing.
Pardis Sabeti: Yeah for sure. March was when they could start doing testing essentially. And then, like I said, from there getting into June, July, people were still waiting for… Nobody was setting up that testing. There’s 260,000 clinical labs, only 200 of them had testing. And the other ones were just calling manufacturers, being like, “Where are my kits?” It’s crazy. That cannot happen again. And in the meantime, the virus didn’t mutate just once, but twice, and three times, and four times. It picked up speed and we were not…
Rob Wiblin: …it keeps getting more contagious.
Pardis Sabeti: Yeah.
How this technology could apply to the US [01:06:41]
Rob Wiblin: The SENTINEL system that I saw from 2019 was focused on countries like Nigeria and the DRC, I guess because of their background dealing with hemorrhagic fevers and the serious contagious diseases that they have there. But presumably things will be a bit different in a country like the United States. I’d like to maybe think about how these ideas could be applied to the U.S. for a bit. The Advanced Molecular Detection program at the U.S. CDC was recently awarded $1.7 billion for sequencing in order to build proper, enduring capability to prevent pandemics, and potentially bioweapons attacks as well. Which seems really fantastic because for reference its budget is usually $30 million. So it’s a substantial scale-up of that program. If you were making a plan for controlling a pandemic in the U.S., how would you spend that kind of money?
Pardis Sabeti: That was very welcome news. I wish we had had this at least early in the outbreak, but I understand why the government prioritized some of the things that they prioritized and so I respect that. And the mRNAs were very successful and so I’m happy about that. But I think it’s one of those things where I understand why they prioritized what they prioritized, but all of it was necessary. And so they could have also prioritized this earlier or pushed it forward. But I think that they’re doing the right things. They are creating centers of excellence and research centers to push this technology forward. And a lot of the big advances in genomic technologies, both from the experimental side, the sequencing and the different kinds of technologies, as well as the bioinformatics, the tools are coming out of academic centers.
Pardis Sabeti: And so you want to support those academic centers and give them significant investment to move that forward and to be able to scale this technology the way it needs to. But then you really need to build that capacity into the public health system. And so we’ve been working actually with the CDC for about the last five years. Through the CDC and the Massachusetts Department of Health, we had a program where we had folks from the CDC as well as eight departments of health come and stay with us at the Broad Institute where I work. And we had two different week-long programs, one in genomics and the other one in bioinformatics that they all participated in year after year. And it was awesome. What was really great about that is it’s through this coordinated education that you also can get coordination.
Pardis Sabeti: Basically the way we designed that curriculum was as experiential learning. We had people bring their own, in the first instance, rabies samples, hepatitis we did later. But in the first instance we said, “Okay, everyone has rabies in their backyard, bring it here. We’ll all sequence them here at the Broad. We’ll collectively analyze it together and we’ll look at a map of what’s happening with rabies.” We started the program in the New England area. And then we were expanding that program across the country when COVID hit. That was really a fulfilling experience and really wonderful to work with the departments of health. One of the things I learned about spending time with folks from the departments of health across the country is that they’re really terrific humans who really want to make their states and their countries and their planet better.
Pardis Sabeti: They’re usually really under-resourced, and have a lot of competing demands, and are getting switched off of things so often. And what was really tough about that is that year after year, they learned this technology and they were really well positioned and then we’d sort of try to keep doing it and they’re like, “Well, our budget for sequencing is essentially like 20 samples.” And you’re like, “Well, what are we training you for if there’s no resources to actually do anything with that?” And so that was always really tough. And so I think that hopefully it comes with that broader education, that kind of coordinated education across the country so that everyone is speaking the same language and has the most advanced tools at their fingertips, but then is coordinated in sharing information. There’s a lot of things that also need to happen around how we quickly share this very sensitive but very important data.
Pardis Sabeti: To answer your question, it would be supporting the academic centers so that they can advance the technologies and serve as resources to public health units, and be able to also serve research capacity and follow up. What often happens with departments of health is that they have to worry about the next problem. So supporting those departments of health to do more testing than they’re doing now and be able to do that surveillance is important because they are the frontline. Those are the two key pieces, and then really the bioinformatic tools to connect all that information in real time. And that synergy of getting that data connected to really important metadata that would enable us to make more meaningful conclusions from what we find, but do so in a way that protects the individual. Gives as much visibility as you can while still protecting the individual.
Pardis Sabeti: And that’s a dance. You have to know what’s going on with the virus. It’s very interesting: This data becomes the most sensitive, but it’s one where we need it the most in real time. We need to know where the person that might have Ebola is going, but we also need to give that person freedom. I guess ultimately one of the things you have to build into it is trust. So how do you create systems that build trust and sustain it and earn it? Funding also needs to be put to that to make sure that’s done well, because the whole system collapses if you lose that.
Rob Wiblin: Do you have any idea how much it would cost to cover the whole U.S. population, or close to the whole U.S. population, with a diagnostic system like the SENTINEL one? Is that something that’s within the potential budget of U.S. federal government and state budgets?
Pardis Sabeti: Certainly. Yeah. The fact of the matter is if you think about the budget that we spend, diagnostics are such a tiny part of the cost. What’s remarkable about COVID is that we had a tremendous amount of testing that we were doing. But we just tested the privileged people over and over again, instead of testing people who needed it when they needed it. Another paper that we put out was called The Case for Altruism in Institutional Diagnostic Testing. It called out a few pretty remarkable examples, but it was what everybody was doing. I think one example was that the NFL spent $100 million testing 7,000 of their team members and employees over and over again. $100 million just testing members of the NFL. I think it was about 1 million tests, which found a few hundred cases…and still did not stop outbreaks.
Pardis Sabeti: Meanwhile, the communities around them were burning to the ground and people weren’t getting tested. It’s not just the NFL, everyone did it. Every school did it. If we use tests smartly, it’s such a small part of the budget. I don’t know the exact cost, but it’s definitely… Compared to what we spend on overly patented and overly exploited drugs for a lot of these diseases, it’s still a fraction. It’s going to be very economical, particularly for the amount of morbidity and mortality costs and hospital costs. I don’t know the exact numbers, but I do know that we were clearly happy to spend quite frivolously during this pandemic on the testing that we did do.
Rob Wiblin: It seems like maybe the easiest, most practical way that things actually might go is that you would build out a system like this in a country with a unified health service, like the NHS in the U.K., which can potentially just say, as a matter of policy, this is going to be an important way that we’re going to spend our money is to have diagnostics in all of our different facilities and operate this SENTINEL system and pay for it. And I guess also not do it over two years, but do it over 20 years as this technology matures and becomes cheaper. And then it doesn’t stand out as a massive expense. It just starts to seem obviously the natural thing that you would do as part of your diagnostic system to deal with contagious diseases in your country.
Pardis Sabeti: Yeah. And I don’t think it needs to be 20 years, but it could be over the next five to 10 years.
Rob Wiblin: I guess in the U.S. to cover everyone, are we thinking $10 billion a year or something like that? Is there any way of giving a sense of the magnitude?
Pardis Sabeti: I haven’t done the economics of it. But a lot of the tests could be as little as a couple of dollars. The other big issue is that depending on how you’re doing it and who’s doing it and where, the economics will change a lot. That same paper that we published, that policy piece in the The New England Journal of Medicine, it talked about the fact that there were not enough labs setting up testing, but then it just talked about the extraordinary amount of price gouging that was going on. We had a couple flagrant examples where we showed that people were charging $2,000 per test.
Pardis Sabeti: Personally I had to pay several hundred dollars for a test. But there are tests that you could do for about $5 a test. And then you have to just decide to do that. Figure out what tests there are and which ones you could use and how cheap you could get them. You could get them to dollars per test. And then figure out who you test and how you prioritize that. The more information you have, the more community buy-in… If you’re looking for particular infections, the more you have a sense of what’s circulating, the more directed you can be with the tests that you run. And so I think the pieces of information I don’t have are how many people are sick per year. I know it’s a large number.
Rob Wiblin: …how many tests you’d need to run.
Pardis Sabeti: Yeah. And also because right now there’s so many people actually coming and asking for tests, but that’s actually probably a small fraction of people that would do it if there was a test for other things. Most people don’t go to the hospital because there’s no test. I think getting that collective information… Again, the cost is still going to be very small relative to the lost labor, life, hospital time, all of those things. Yeah, I would welcome that calculation being done. And I’m happy to do it myself, I just haven’t done it in preparation for this meeting.
Rob Wiblin: Right. You’re trying to get it actually scaled up and working and working in specific places. And I’m like, “How much would it cost to do the entire United States? What about the whole world?” It’s easy for me to ask, I guess, because I’m not going to actually have to do it.
Pardis Sabeti: It wouldn’t take long to come up with something, and I’m certain that it would be economically sound to do.
Rob Wiblin: Yeah. I guess probably the answer is also no to this one, but has anyone done a cost-benefit analysis test? I guess economists have been doing this for the COVID-19 responses and saying all of these COVID-19 actions, paying for vaccines, paying for testing, they pay themselves back like many, many multiples. It’s just so obvious that we should be spending on this because it’s so much cheaper than requiring people to just stay at home. And I guess a similar logic might apply to this. There might be a significant up-front spend on all this diagnostic machinery or all of the materials, but then you stop pandemics that can cost you 10% or 20% or 30% of GDP and that can kill enormous numbers of people. So the return on investment might be very high.
Pardis Sabeti: Yeah. I think that’s right. I think a lot of people have made the economic case for this in great detail. And I think that even just this one pandemic, the cost of it would pay for the next 20 years of what we could have done to stave it off. The interesting thing is it’s probably still economical on an annual basis, it probably is beneficial. And then when you think about the pandemic it might stave off, it’s a no-brainer. It’s a tiny, tiny fraction of what the costs can be to society.
Pardis Sabeti: For example, Ebola cost $42 billion to those local economies. And that was only about 30,000 confirmed cases. You can see what the impact is. If any virus gets out, it will devastate an economy. So having a system in place to pick it up is key.
Failure modes for this technology [01:18:34]
Rob Wiblin: I’d like to put a couple of critiques to you on how practical this whole system might be, or ways that it might potentially fail or struggle. If this whole system were put in place, what would be the most likely way for it to fail or not achieve as much as you’d like, if you had to guess?
Pardis Sabeti: Yeah, we’ve thought about this in varying ways. There are many different failure modes for this technology. Misuse will be a really important thing to watch for, because a lot of the technologies… We haven’t talked about the fact that things like mobile applications and Bluetooth and geolocation, all of those things are also really important and will be beneficial to a system, but have so many potential misuses. I think probably the single biggest challenge to the use of this is protecting against misuse. And at the end of the day, viruses are insidious deadly threats that weaponize your neighbor against you, and if we don’t manage that well, people can get pretty hysterical. And we’ve seen it with HIV, with COVID, with Ebola, so many different cases in which the culture becomes very toxic.
Pardis Sabeti: And so that’s one of the things that we try to build into everything we do. What’s important is this idea of making sure that the systems we put in place are ones that are thought through with regard to how they work for the communities. And that every potential misuse is considered. If you want to really stop a pandemic, you need incredible amounts of visibility. And it’s really challenging when you have all of the next generation of kids out there on TikTok and Instagram and all these places sharing all of this really personal private information with no problem, but then when it’s your location as it relates to potentially spreading COVID amongst the community, nobody wants to talk about it. There’s part of me that’s like, what’s going on here?
Pardis Sabeti: You’re literally giving away the most personal private information, but yet the thing that could actually save a life, you’re afraid to share. But at the same time, there’s a reason for that. It can be so stigmatized. And so what we’ve been doing is we’ve been piloting these types of technologies in very specific settings. When we started developing it, we were developing it for Harvard at Harvard. And the way I pitched it is the Facebook app for outbreaks, that starts within a close-knit community. A place where you can test and see how things go and get buy-in, local buy-in, and show utility to people. But Facebook can be co-opted in all sorts of bad ways, so it has to be protected and nurtured at every step.
Pardis Sabeti: And so I do think that it is about showing the use case in some environments in which there is trust, and then being able to then roll those out to other places while maintaining that level of personal-ness. I often say public health needs to be local. You can’t have somebody in Washington trying to figure out what went down in some school somewhere else. The local janitor will have more information about things, like, “Oh, well actually there’s this bathroom that everybody uses.” You actually want to empower every single person on site to be able to do this in the right way with people they trust, and in a way that builds trust.
Pardis Sabeti: There are many, many challenges, but that’s probably the one that’s foremost in my mind. How do you build these technologies? And how do you roll them out in a way that they are used well and where we remember that the virus is the threat, not each other? It is tough. And I think there’s a lot of work we have to do to build trust in society broadly in order to get there.
Rob Wiblin: When I was trying to envisage the SENTINEL system being scaled up and was thinking, “How might this go wrong?” It all came back to just logistical and scaling challenges. It’s just so hard to build big programs that work really well, that involve coordination of so many different groups. I guess whether you’re doing this in Nigeria or you’re doing it in the United States, it seems like this is going to require coordinating with tens of thousands of different medical centers, potentially hundreds of thousands of different staff who are going to have to learn these new programs and figure out how to send this data.
Rob Wiblin: The IT system, especially across the U.S… It’s such a fractured medical system. You’re going to have to get all of these people figuring out how to send all of this data to some central place where it can be analyzed. As I understand it, many medical centers in the U.K. and the U.S. they’re struggling even to get electronic records of just people’s people’s GP visits. Medical IT just seems to be an extremely difficult area. There’s just all of these practical hurdles that I imagine can be overcome, but it’s going to require real expertise and serious work. Is that something that concerns you as well?
Pardis Sabeti: Yes. If you really are going to try to scale this across the country, it’s daunting. But I always talk about how Coca-Cola somehow gets their Coke bottles to the most distant village… In the middle of Ebola we’re trying to figure out how to get PPE to people and somehow you see the Necco car going by. Whenever you incentivize it in a capitalistic way, people find a way. And so I think that’s what we need to do. The only thing that could bring people together against a common enemy in the same way as this is an alien invasion, so ultimately this is a moment… If we can’t collectively solve these problems, that’s on us.
Pardis Sabeti: Of course it’s challenging and it’s huge, but it’s exactly the thing that we need to do. You’re right. The medical system is really fractured in this country and it’s really hard, but the infectious disease medical system can be pretty contained, and that one piece could be managed and organized and solved. And then in doing so it can create an infrastructure that can be the backbone of other care for people. I think it’s one of the most important things that we could do, and I think if I have the opportunity to speak to people in government through this podcast, this is the moment in time to invest in building out a medical system that is more universal and that could have a broader impact in healthcare.
Pardis Sabeti: And what’s nice about it is when you think about what you need to do to solve an outbreak, it crosses clinical medicine, statistics, epidemiology, public health, policy, psychology… Every part of it you need to understand and you need to get right. And if you can, you’re building a robust system that has applications to a lot of things. When we talk about precision medicine, the most precise thing is just finding a virus in your system. And so it’s a starting point for all of the things that you need to do and build to build a robust healthcare system and a connected society. I think it’s a challenge, but it’s a challenge we should embrace.
Rob Wiblin: Yeah the SENTINEL system involves coordinating tons of people. Is there any way of shrinking the number of people who can be involved? Andy Weber envisaged this lovely futuristic scenario where everyone has this kit in their house, the gene sequencing kit, and that has this nice cleanness to it. It’s like everyone’s using the Amazon Echo or something, and it all just gets sent through the internet to this central repository held by a private company, I suppose. And then it could all get analyzed there and then other people don’t have to be involved. You can just ship it out in the mail. Do you think there’s any way of potentially simplifying it, where maybe this can be slightly cordoned off from the rest of the medical system? Or is that just the kind of thing that someone like me who doesn’t understand what’s going on would say?
Pardis Sabeti: Yeah, it could be, it certainly could be. Because that’s the thing, you don’t need all of people’s medical information to solve this one thing. And one of the big impediments to doing this work is that it went through a lot of immigrant communities and there are a lot of undocumented people in those immigrant communities who didn’t want to come to attention. And when we build the system, we don’t need to even build a system where we have access to you long term, or to your information. There’s a short period of time where you are a person of interest, you are carrying a virus or have been exposed to a virus that we need to watch, but we can just give you a burner phone that we use to contact you just for that period of time. And then you can go off the grid.
Pardis Sabeti: So I do think that is an approach that’s a viable one, of making it a system that’s outside of the general medical system and that is only related to what we need to know for a particular pandemic threat for a particular point in time.
Funding [01:27:06]
Rob Wiblin: Let’s push on and talk about funding for programs like this. Ideally we would like to see this kind of system, this diagnostic system, set up in countries all over the world. Who is best placed to fund these kinds of pilot programs and then to scale them up? Is it national governments, or are there international organizations that should be involved?
Pardis Sabeti: It’s probably both. What we found is that in general a lot of the governments move really slowly, so there is a real place for philanthropy early in the outbreak to move these things forward. That said, philanthropy is a dangerous thing because it means that a small set of people get to make a decision, often in conversations that happen in back rooms and that don’t have a merit base. So one issue with the philanthropic version of this is that certain people got chosen and certain people didn’t, and a lot of people who had a lot to contribute didn’t. Philanthropy is really powerful and it allows people to make those kinds of moves that you can’t in a bureaucratic administration, but it also then does anoint the few that get to respond, and we need more voices.
Rob Wiblin: Yeah. There also just isn’t enough money in philanthropy to scale these things. They can take the risk of testing it out, but…
Pardis Sabeti: That’s right. But they can definitely help move the needle, and they can help in quick moments of crisis. Then it’s national governments and international organizations where possible. And then there could be an economic model, right? If you are a company like Amazon, or big oil companies where you have a lot of employees that are in regular contact with each other, there should be an incentive to keep them healthy.
Pardis Sabeti: I mean, I know a lot of these companies are just happy having people falling ill and coming in, but there is lost productivity there. And there’s definitely a lot of lost life and a lot of pain that’s unnecessary that’s inflicted on people. But even if you’re still forced to go to work, there’s lost productivity when you’re just not at your peak. And so ultimately I think that we can also push for having a private industry supporting this.
Pardis Sabeti: What is remarkable about COVID is that people spent a year not getting sick from the flu and not getting sick from a lot of other things. And then they realized — even though the circumstances were bananas — how much more productive they can be if they’re not sick all the time. And so there is a very specific, clear economic case that can be made. And I think that you could have private industry playing a part in supporting their communities to do better too.
Rob Wiblin: Yeah. I guess this isn’t really ideal from a public health point of view, but if these tests get cheap and easy enough, then you could have a direct-to-consumer model where you have a company that manufactures them and sells them to people, potentially for not that much money. And then they send them back in and then that company can collect and use that data. You get to take advantage of the fact that lots of people are willing to pay because they’re really curious. Like, “Why am I sick? What have I got?”
Pardis Sabeti: Totally. Yeah, that’s exactly right. And it may well be that the solutions just come from that commercial interest, because people have obviously paid a lot more for a lot less beneficial things. But yeah, I think that probably is where it will go. And you’re already starting to see it during COVID where people are paying just to get at-home tests and all these kinds of things. So when it gets to the point where it’s cheap enough, it just might become common. The question there is though — like you said, so often that information ends up going into a private company’s databases. So how do you make sure that we share that information, even if people are using different systems? Make sure that information is collected and shared in a way that’s useful for all?
Rob Wiblin: This does to me highlight one advantage of having a nationalized government healthcare system like the NHS. I mean, I guess they have struggles systematizing and uniformizing everything internally. But it’s a lot easier for them to do that than a country that has 50 different states running 50 different healthcare systems, which is then also broken down into all of these private companies.
Pardis Sabeti: Certainly, I think it’s more than that, right? I think even within the states, each county has its own healthcare system where often they don’t share data amongst them. So certainly pandemics make a really strong case for a national health care system.
mRNA vaccines [01:31:14]
Rob Wiblin: Let’s push on and talk about mRNA vaccines for just a minute. Andy seemed to think that these diagnostic methods would be extremely complementary with mRNA vaccine technology, because using… So the third stage of the diagnostic is the gene sequencing, and then using those sequences, you could potentially immediately get the sequence of any new disease. Maybe even before you know that it’s the new disease, you’ve got the sequence. And then you can start working on an mRNA vaccine candidate the same day, potentially. I don’t know whether it was Pfizer or Moderna, but one of them basically had a 24-hour turnaround between getting the sequence and having their vaccine candidate. I think the one that was actually successful, ultimately. Is there anything important to add to that picture, or is that just right?
Pardis Sabeti: So mRNA vaccines are part of a class of things that we call programmable technologies, programmable countermeasures. When you target the genome sequence of a virus or any kind of microbe, it’s an input that is very easy to swap out. And obviously there’s certain things you’re going to want to know about, which part of the virus do you want to target and what exactly do you want to do? And so those vaccines did benefit from the fact that people who had been looking at SARS-CoV-2 beforehand had a sense of what part of the genome was going to stimulate the immune response the best.
Pardis Sabeti: I think they probably even had a few lucky points with the fact that some of the things that they did, they did some optimization that could have had a negative impact, but it worked out in this setting. So it’s not as easy as any virus immediately, you would know, but it can be very, very rapid. So I think it’s just, if the viruses start getting really different and we don’t understand as much about them, we just may not know exactly what to target. But I think we will get to the point where it can look like that futuristic thing you’re describing.
Rob Wiblin: It occurred to me that it would be really neat to always have a pre-approved mRNA vaccine trial just ready to go with willing patients lined up, just ready for the next time that we identify a new disease. Because then you can get the sequence, not in 24 hours necessarily, but pretty quickly you come up with your vaccine candidate, and then hopefully you can manufacture them really quickly and start injections within a week maybe. And I think with SARS-CoV-2, it took them two months from the vaccine candidate to actually starting the trial. So maybe we could save a month, something like that, by just having the trial and having everyone sitting there ready to go. Does that sound right?
Pardis Sabeti: Yeah. I mean, I think that one of the things, as much as the specifics of the particular SARS-CoV-2 vaccine was important with what happened here, it was just the trying and testing of mRNA vaccines in general. And seeing that there was no negative outcome, at least reported so far, of just using this kind of technology or the liquid nanoparticles that they are injected with, none of those were causing serious side effects, or at least not enough to stop it. So we were already very well positioned in that case where the impact we’d be looking for is the impact of a particular sequence we might inject, but not necessarily the technology.
Pardis Sabeti: So I do think that we’re at a place where it could go much, much more quickly. And you’re right, much of the delays… We often like to show a Gantt chart of how long things we do take. And a lot of the delays are administrative or bureaucratic or something kind of… Something that could be shrunk with better processes and better operations management. So having clinical trials ready to go and people poised and ready I think would be yet another thing to shave time.
Rob Wiblin: I know there’s people listening in the U.K. and U.S. government, so please spread the word about that idea. Let’s have the volunteers ready to get on the phone as soon as we find the next pandemic.
Other emerging technologies [01:34:45]
Rob Wiblin: Let’s push on and talk about some other technologies. We’ve talked about three things that I’m particularly psyched about here, but I know there’s a lot more going on in your lab, and of course in the broader biology world. What are some other emerging technologies that you think could play an important role in pandemic control, that it would be useful for the audience to know about?
Pardis Sabeti: There’s a lot of different technologies. Two really big areas, the first is monoclonal antibodies or just antibodies in general. Essentially you read out what is the host response to a particular virus or particular microbe, and then design antibodies that essentially mimic that. All of these things are usually in some fashion inspired by or identified in nature, but basically in a lot of previous things where people didn’t have many ways to respond to infectious disease spreads, people would use convalescent plasma.
Pardis Sabeti: They would just take somebody who got ill from an infection and recovered, and then just use their plasma to then make others get better. And they found that it worked. They found that basically the blood from somebody who’s convalescent, who’s recovered from an infection, will carry antibodies. And those antibodies can act in somebody else and stop the infection, or buy time for the person to mount their own response. And so that’s really cool and powerful. Obviously it can’t really be scaled, and there’s a lot of ethical issues and lots of ways that that ends up going haywire, but that basically has inspired a whole area of therapeutics that is basically saying, “Okay, can we read that out and can we make synthetic versions of that?” And so that was really important during the Ebola outbreak. And there’s been more work on that too. Regeneron — what President Trump got — that technology is based on that premise.
Rob Wiblin: Okay. So the idea there is that your adaptive immune system produces these antibodies, but it takes weeks potentially to really scale up and produce enough of them. So what if you could just get an injection that had those antibodies, or something very similar to the antibodies that you’re ultimately going to produce, and you could get a whole injection of them now, and those would connect to the virus particles of the pathogens and then they’ll get eaten by the immune system. We do have a very expensive and difficult method of getting antibodies, which is to find people who’ve just recovered from the disease and extract it from their blood, but it’s challenging and we’re not going to be able to produce enough on cue.
Pardis Sabeti: Yeah. And you can imagine lots of ways that that could turn into a really dangerous thing, when people are starting to grab people who are recovered. Yeah. All sorts of messy.
Rob Wiblin: Yeah. So the challenge here is the manufacturing, I’m guessing? But are we making progress on figuring out how to just make these in a lab?
Pardis Sabeti: So this is actually not an area I work in, I should say, but this is an area I’m very interested in. But DARPA has a big program around getting these to be able to be manufactured much more quickly. And you said that a lot of the manufacturing used to be hard and it would be done in these model systems that were cumbersome and so very expensive to manufacture. But I think that’s where the investment is, how to get them to manufacturing scale.
Pardis Sabeti: Another example, we talked about the fact that CRISPR came from nature as bacteria’s immune system to viruses and it’s designed in nature to detect and destroy viruses. And so whenever you find things in nature, it’s good and it’s helpful because you plot what it’s already doing. So they’re very good at destroying viruses, but they weren’t really designed in nature to do it in mammalian cells, to do it in human cells, and in big humans.
Pardis Sabeti: So there’s a lot to take it from here to action, but there’s a lot of interest also there. And so my group has done work on that. And these are all technologies that are again, programmable, where you know a sequence and you could immediately within a day plug in the new sequence and knock it down. In our lab we studied influenza, VSV and LCMV, which is another arenavirus like Lassa, and showed that in mammalian cells, we could knock down those viruses and decrease infectivity by several hundred fold using these guides. So that’s really powerful.
Pardis Sabeti: We can use them in mammalian cells, but then the next challenge is how do you get them in the whole organism and get them to where they need to go, and what are the off-target effects and all of that. So there’s a lot to go from here to there, but that’s another really interesting area. Another big player in the space were the adenoviruses. They had a little bit more of a complicated spell, and there’s some issues there with using a DNA virus to make a vaccine. And so we’ll see where that goes, but there’s a lot of work happening in making these recombinant viral vector vaccines, so that will be another interesting thing to look out for.
Pardis Sabeti: And then from my own side, it’s all a lot of those detection technologies. And so we work very closely with an amazing firm called Fathom Information Design. Ben Fry is the founder of Fathom. Ben is the person who all of my most genius computational friends say is a genius, and who can make computers do whatever. But he basically created the language processing that is used by designers all over the world to make data look like magic and do extraordinary things. We’ve been partnered with him for a long time, building out these systems for dashboards. Basically every time I show people the dashboards Ben’s made, they’re like, “Oh, that’s the future.” Ben’s stuff was used in Minority Report and in The Hulk, 20 years ago. When people showed what the future looked like, it was what Ben developed. It’s really beautiful. I mean, those rapid analytics are going to make a big difference.
Pardis Sabeti: And so we’ve been building these systems that let public health people really track, “Where are our cases coming from? Where could they be circulating?” And then thinking about how to tie that to information that people share about their contacts. We’ve actually been building a lot of Bluetooth-type technologies for a long time. We were doing it with these small communities with people sharing, and now in COVID it was like you know what, let’s make all the contacts manual and have people report them, or be the ones that the schools are reporting. But that information is fairly powerful and important. So I think those technologies are also going to be really valuable.
Operation Outbreak [01:41:07]
Pardis Sabeti: So we’re really invested in education, and we do a lot of frontline/scientist/genomicist/department of health education, but we also do a lot of kids education. And in 2015, Todd Brown who’s a civics teacher at Sarasota Military Prep Academy, a charter school in Sarasota, Florida, reached out to me and asked me to Skype with his students and then we hit it off. And then he wanted to build a civics curriculum around pandemics for seventh and eighth graders. And Todd’s amazing. He’s now a BFF. We are sort of ride-or-die for each other on all sorts of projects, but basically through this, he brought up this program we now call Operation Outbreak, which is a curriculum in pandemics for people of all ages, that ends with a simulation. You don’t need the curriculum to do the simulation, but it’s helpful.
Pardis Sabeti: Essentially you simulate an outbreak and then you have to respond to it. So Todd’s students were amazing. Essentially about 200 students, seventh and eighth graders participating in full PPE, body teams, a media team, the government team, the whole nine yards. I mean, full realism, really amazing images that you get of them creating a pandemic and responding to it. And what was sort of neat is at the same time that we were helping advising on that, Andrés Colubri, a postdoc in my lab, was building epidemiological models for outbreaks on college campuses where we were investigating an outbreak of mumps at Harvard and building Bluetooth technologies to track outbreaks. And through these conversations with Todd, we ended up basically having him build an app that spreads a virtual virus via Bluetooth. And so you could mimic full outbreak events.
Pardis Sabeti: And so that was like the missing piece of the realism for our outbreak. It’s just, how do you spread this virus? But basically it’s on the kids’ phones and there’s all these emojis where you’re sick and you’re vomiting and all sorts of things are happening and you can unlock diagnostics and see whether or not you have the thing, and you can use vaccines. So we could almost mimic every part of the outbreak and mitigation strategies. We even had beacons, like a dirty sink that was emitting the virus. And so really it’s pretty awesome. We got to the point where we had a full-fledged outbreak and we even created an economic model so the kids couldn’t just hide. They had to come out and get stuff. So there were all sorts of those pieces we put together and we’ve been rolling that out.
Pardis Sabeti: And Ben and the Fathom team have developed this dashboard, where again, it looks like the future. Students can see what happened in their simulation and they can look at the data and they can understand all of the different pieces and investigate it. So I think that’s another thing that we’re really excited about is at the very least, we should have involved people more in the COVID response, as opposed to being like the government’s got this, wait for us. I think it would have built more trust if they had more agency. But also even if they didn’t, why didn’t we at least use this as an opportunity to teach them about genomics and public health and epidemiology and what R0 is. I mean, there’s so much math and science that we could have taught them and got them to be more participants in contact tracing in a positive way and the psychology of it and all of that.
Pardis Sabeti: We’re now working with the department of education of Louisiana, and they are going to be doing a curriculum for all 11th and 12th graders that is voluntary, but it’s an elective curriculum they can do that will basically use our operations, our outbreak science textbook that we’ve developed. And then the students will get to participate in these simulations. So we’re pretty excited about it. And we’re excited about empowering the next generation of scientists. But we’d also love to come down to DC and run it at Congress. People need to understand, what does it look like? When we say R0, what’s going on? All of those things. There’s nothing that can beat experiential learning, ideally not in a life or death situation, but in a game you can actually see all of these things. So that’s another piece that we’ve been really invested in and excited about.
Rob Wiblin: I wonder whether people might be interested in playing this as a game, as an app on their phone to see whether what they’re doing is safe enough that they wouldn’t catch the virus. You could imagine lots of people in London, where I live, playing this, and then you’ve got to try to avoid catching the virus on the tube and things like that. And you get some indication of how much risk you have actually been exposing yourself to, which is so hard to judge.
Pardis Sabeti: Totally. Right. Because most of the time you play these things and you’re giving the data to somebody, but then you’re not getting it back. We thought, you know what? The game is the way we actually solve it, people just want to play a game. And meanwhile, a real virus happens. You just turned it from a fake virus to a real virus. Right? So yeah, if there’s any gamers out there, we’ve been in touch with some different groups, but trying to sort of say, how do we actually turn this into a collective collaborative game.
Pardis Sabeti: And here’s the thing, most people know how many contacts they have every day. Right? But they don’t know how many contacts their contacts have. What is your true exposure? Your buddy down the hall, who else has he been with? And it’s remarkable. I would love to get to show you the visual. If you go to operationoutbreak.org, you can see a visualization of one of our cases. But you see most people social distancing most of the time. And then there’s a few people that have 70 contacts. And then every person who’s in contact with one of those people essentially—
Rob Wiblin: …is toast.
Pardis Sabeti: Yeah. And so it is pretty neat to get a real sense of what is my actual exposure? And there’s a funny meme where it’s like, what you think your bubble is and what your bubble really is. And this really shows you that.
Rob Wiblin: Yeah. I would have been really fascinated to see that during this pandemic, to have a good sense. It’s like, yeah, when you decide whether to meet up with someone, you’re going to ask them “What have you been up to this week?” You always wonder, are they telling you everything? Are they remembering everything that they’ve been doing? There’s definitely a temptation to not mention that thing that you did eight days ago that might’ve been a little bit dangerous.
Pardis Sabeti: And that is the challenge, right? My dad was the director of intelligence of SAVAK. And I spent a lot of my childhood in hiding, so I have this… Everything that I think of is a nice idea, I think, “Who’s going to co-op this in which way, and how’s this going to go?” Right. Because then you’re like, you’re trying to figure out where somebody you like, your ex-girlfriend, where they are. There’s all sorts of ways that somebody is going to try to use this in a really bad way. How do you figure out how to get people the information they need, and nothing else?
Pardis Sabeti: But in the game setting, particularly when they could turn it on for a little period of time, you can try this and understand it. That’s what we like. We are working in a college in Colorado and we let them do it for one week. And so for that one week they could know, hey, they’re being tracked for that one week, they’ll get a sense of what’s going on. And it’s pretty remarkable. That’s where they found some people had 70 contacts. And so you can find that information and you can do it anonymously and you can get them that insight without too much exposure. Tiptoe into it and figure out all the ways it can get misused bit by bit, without rolling it out and then finding out all the ways it can be co-opted.
Rob Wiblin: Skipping back to the biotechnologies you were talking about, I guess the important thing to note and the reason that you wanted to mention those things probably and why they’re so cool is that they’re all platforms that can be applied to tons of different pathogens. It’s just so much more useful to develop a platform, a diagnostic platform, or a vaccine platform, or a treatment platform that can apply potentially to a large fraction of all pathogens than it is to develop one that’s boutique and specific to just one. And it seems like that’s a big area where humanity could invest more, is seeing the bigger picture and realizing we don’t just need to fight this pandemic, we need to fund the technologies that will eliminate disease in general, or contagious diseases in general.
COVID [01:49:16]
Rob Wiblin: Let’s push on and very briefly talk about COVID. Are there any things that you’d like to see the U.S. or U.K. governments do about COVID that they’re not already doing?
Pardis Sabeti: Well, the U.S. is a very interesting place. When you go outside, people are starting to act like this is behind us. Vaccines do work, and cases are plummeting across the country, and that’s all really great. But the fear I’ve always had since the beginning of this outbreak is this complacency with this idea of it only affecting the older and infirm. And of course that’s not great. We don’t want those people to be at risk either, but there’s also a complacency with the belief that it couldn’t affect younger people. Right now, individuals who are younger than 12 still can’t get a vaccine. And the virus has changed, and at any point it could start affecting children. And so we really do need to actually keep up the work to try to root this out. The only way that you’ll know that a virus isn’t going to change in an unanticipated way is to get it to zero.
Pardis Sabeti: And so that’s why we should not feel comfortable until it’s at zero. And not just the United States, but anywhere in the world. I think that there is more and more of a push of supporting other countries, but viruses do not respect boundaries, and no matter what isolationist tendencies you have, it’s never been effective in stopping outbreaks from happening. And usually in fact it makes it worse, because there isn’t more communication across countries. And so I would say where countries that have it under control should focus is getting their own cases down to zero and helping other countries do so as well. It’s really terrifying to see what’s happening in places like India right now. Both for those individuals there and the harbinger of what that can mean for us.
Pardis Sabeti: We sat complacently in the United States back in February of 2020, hearing these transcripts from places like Italy of what they were experiencing. And it was only going to be what was going to come to us later. We are seeing, in a lot of different places, more and more evidence of illness in children. We should know that that is likely going to come to us if we’re not careful. And I think about that in particular. Kids gave up so much of their lives last year to protect the older generation. And we honestly should do the same for them. If they can’t be vaccinated… I have gotten a vaccine, but when I thought about getting one, it wasn’t because I wanted to protect myself. It was my responsibility to do that for other people who can’t get vaccinated for varying reasons.
Rob Wiblin: You mentioned earlier that this research that you did, where you were looking at if you’re a group, I guess a university or a sports league, and you want to make sure that a pandemic doesn’t get in to your group so that you can continue operating normally, at some point once you have enough tests, then it’s actually much more efficient to give them to your neighbors or the people that you’re living with, or people who you’re potentially socially going to be exposed to than to just test your own people even more. And that makes some intuitive sense, because of course, the only way that you’re going to be penetrated with a pathogen is exposure to someone who’s on the surface of this, who’s on the boundary of this group. And after a while, you just hit really diminishing returns, testing your own people even more often.
Rob Wiblin: But yeah, in the paper, you mentioned it’s interesting psychologically that most groups haven’t been interested in doing this. And I guess most countries also haven’t been that keen on sharing their tests. And it seems like we see something potentially similar… Maybe it’s too soon to say, but it does seem like countries are not that excited to spend money buying vaccines for other countries, or share them with countries that might struggle to afford them. Even though I saw this paper from the IMF last week where they were saying it is actually profitable, outright profitable. It requires no altruism to justify the U.S. buying vaccines for really poor countries, because the U.S. profits in a bunch of different ways. They don’t import the virus back if it’s not in other countries. You avoid new strains appearing that then might be immune to the vaccines that we’ve gotten, just recreate the problem all again, or might be more virulent or affect children, as you’re saying.
Rob Wiblin: And also of course, if other countries are doing well economically, then they’re buying and trading with the United States. And so you’re making money that way. And just the return on vaccines in general is so great that even if you’re a different country, you benefit from another country getting them. But despite this logic, it’s so far been hard to raise money internationally to get the world’s poorest countries vaccinated. I think and hope that this may change as vaccines become more abundant and countries are thinking less about how to vaccinate their own populations and then can think more about how to vaccinate the world. But it does seem like we have this inward-focused view.
Pardis Sabeti: Totally. There’s always that debate, are humans inherently selfish or selfless? Kids can be pretty selfish, they’re like my toy, my thing. There’s all these things that make people regress, and I feel like outbreaks are something that make people regress. I think people always have this feeling that in an outbreak everyone’s going to appeal to the better angels of their nature and become better humans. And it’s like, no, they’re punching each other in grocery stores and they’re fighting over toilet paper. And why would you expect something more than that? You’re saying there’s an insidious, deadly threat that’s weaponizing your neighbor against you, turning them essentially into a zombie, somebody that can affect them.
Pardis Sabeti: And so there’s a natural tendency to become very selfish. And it’s really interesting to watch just how extreme it is. I’m not going to say specifically what places, but I was in a lot of conversations where I was begging people to consider testing outside of their own institutions, saying to them it looks really bad. I mean, just as a starting point, it looks terrible that you’re investing this much money and you’re bringing people back, particularly on college campuses, it’s like you’re bringing people back in the middle of the pandemic that’s going to inflame your local community, but even more so where it’s like you’re taking all these resources. And so finally, when we did the paper about the case for altruism in testing, it was literally to answer that question.
Pardis Sabeti: I kept saying intuitively it makes sense that the more you test other people, the better off you will be, and the more insight you have about what’s going on. But what exactly is the actual economics? What are the numbers there? And it was just a model, just to get started, but it was pretty obvious, every single version of this that we ran, people did better by testing outside. And not just testing a little bit outside, but using the majority of your tests outside. Essentially you’re creating a barrier, right? You’re seeing multiple layers out.
Pardis Sabeti: I’m a math person, so I was really watching how people use data and use it in ways that just don’t make sense. People are always touting their positivity rate and saying oh, this is so great, our positivity rate is so low. But I’m like, that’s because you’re testing healthy people, that means you’re testing badly. The actual true positivity rate is much higher, which means you have terrible aim. And so it’s a very interesting phenomenon when people are so proud to say the positivity is low. If you’re testing positivity is not as good as chance, then you really have a problem. Right? And that’s essentially what we were tolerating. We were tolerating a testing positivity rate that was lower than chance. And so I think that that’s just an example in the diagnostic space of just how badly people had it, but just also how self-focused people become during a pandemic.
Pardis Sabeti: But like you said, what is true is altruism is actually a better model in infectious disease. It just is. Helping your neighbor when they have something like cancer is what you should do as a good person, but it doesn’t actually impact you. Helping your neighbor when it’s something communicable impacts you. And we have to get people to understand that. I would like people to just do it because it’s the right thing to do, but I’m okay with getting them to do it because—
Rob Wiblin: …Self interest is also fine.
Pardis Sabeti: I’ll take it. I’ll take it for now.
Rob Wiblin: Yeah. Keiran just pointed out to me that the Biden Administration yesterday said they’re going to buy 500 million Pfizer coronavirus vaccine doses for the rest of the world, which I guess is about 4% of the total amount that I think is necessary to finish the job. So yeah, that’s really good news. Maybe a sign that now that there’s more to go around in the U.S., we’re going to witness more programs to vaccinate everyone and get COVID as close to eliminated as possible.
Gain-of-function research [01:57:34]
Rob Wiblin: Do you have any overall view on whether gain-of-function research is useful as a part of reducing the risk from contagious diseases in general? Does the benefit outweigh the risk?
Pardis Sabeti: I’m the kind of person that’s very… I see both sides. I see a value in why we should do gain-of-function, and I can see the major risks. And I think that’s the thing, I’ve always myself worked in spaces that are very, very risky. But if you do it, you have to be, you have to always be thinking four steps ahead of what could happen, what could go wrong. And so I think it’s something that there’s a lot of value to do, but I do think that there are real risks and we have to put measures in place to make sure that we mitigate all of those risks at every point.
Pardis Sabeti: And so understanding exactly where a virus can go, whether or not there’s a possibility it could go airborne, whether or not it’s a possibility that it could bind to another receptor and do more harm…. I think this is valuable and it allows us to be a couple of steps ahead of the virus in where it could go. But the possibility of an accidental release or something like that, that can’t be ruled out. It’s possible, and I think that’s where the safety programs really are important, and making sure that there’s a collective universal biosafety commission that makes sure that anybody working on it is doing it safely.
Pardis Sabeti: And then there’s obviously the misuse. As a medical student I sent an op-ed just to The New York Times. It was February 2001 and it was when the human genome project was published. And at that point, the same month that was published there was an article, I think it was in the Journal of Virology, but basically it was this Australian pest control research center. Australia has a lot of pests, and essentially what they have is an institute that tries to figure out how to get rid of those. They’re doing serious gain-of-function research. And basically they published this paper where they showed that IL-4 is an important component of your immune system that regulates your immune response. And if you actually armed the mousepox virus, forgive me if I’ve forgotten, it was 20 years ago, but it was essentially that they armed the mousepox virus with the IL-4 from the mouse, from the rodent itself. Essentially giving the virus this piece of armor from the host immune system that allowed it to knock it down and tell it to go quiet. And it was so incredibly effective that I think it overrode even vaccines and just decimated this population. And it was remarkable and they just decided to publish it to just put it out there that this is possible.
Pardis Sabeti: And there were other papers like that that have come out at varying times. Where there’s like, I think some cat virus also that somebody showed some incredible effects about. And I remembered basically the op-ed I wrote talked about the fact that just as we are publishing the entire book of life that is the human code, we’ve published a paper that shows how you could co-opt that and use it or weaponize it. And so coming back to that point that I made about how we survive our technical adolescence, forget the just innate risks of doing this kind of research, figuring out what a gain of function is is just giving somebody else information about what recipe they want to use in making a virus.
Pardis Sabeti: And so the problem is that they might be doing that whether we do it or not. And so it’s the question of do we just go blind to it and don’t do it, and just hope somebody else doesn’t do it? Or do we do it and do we do it thoughtfully? So I think those are all the really hard questions that need to be asked, and I’ve thought about them in varying ways, but I’m not going to say them here as if they’re fact. I haven’t thought about it deeply enough, but in essence those are the risks. I think it’s important for us to do this kind of research to some degree because we need to be a few steps ahead. But with every step we take there’s the risk of accidental risks or misuse that could be even more damaging.
Career advice [02:01:47]
Rob Wiblin: Let’s move on and talk a bit about advice for people in the audience who might want to have a career a little bit like yours, or just help with the broader project that we’ve been talking about. Your lab has been really thriving and a lot of great people have been coming through it and out of it. Among people in the next generation of your field who’ve flourished, what are some archetypal decisions that they’ve made or practices that they’ve followed?
Pardis Sabeti: In science, so much of your success is built on the success of the community you work with. We talk about the lone genius idea, but that’s just never the case. There’s so many people who are excellent and outstanding whose careers have stalled because of choices that they’ve made. And so there’s so much serendipity and there’s so much luck that goes into these things. But you can build the luck that you have by making really good choices as to where you work and who you work for and with.
Pardis Sabeti: And I think really finding that right community, that both the person and the people that you work with and for have integrity and will look out for you… And it can be a treacherous business, but there are good people out there. And then finding that right place where it’s like yeah, this is the kind of project that I wake up in the morning and think about. And these are the people I want to think about it with. I think my success has been in finding those people and then having the support to do my best work.
Rob Wiblin: What’s one of the most instructive mistakes you’ve made? What can listeners learn from it?
Pardis Sabeti: So when you work in infectious disease and you work on BSL-4 viruses in remote settings, there’s just a million mistakes that can be made and things that can go wrong. And it is about just constantly reacting to it, and learning from it, and digging deep. So there’s an adage I really, really like, it’s from the book Good to Great by Jim Collins, which I recommend to anybody who’s trying to do something great when maybe if they had to be honest with themselves they’re good and not great. The book is based on a lot of really great research, but it has some really good anecdotes that help make the point. And so one of my favorite anecdotes is the Stockdale Paradox. The author is with Admiral Jim Stockdale who is a war veteran, a decorated World War veteran who spent many years in Hanoi Hilton, Vietnam’s forced prison camp, and persevered. And he’s credited with helping others persevere.
Pardis Sabeti: And he said, “How did you do it? How did you survive Hanoi Hilton?” And Jim Stockdale said, “I never lost faith in the enduring fact that I would prevail. I always believed that in the end I would prevail.” And then Jim Collins asked him, “Okay, well who didn’t? Who died there? Who didn’t make it?” And he said, “The optimists.” To which Jim Collins was like, “It sounded like you’re an optimist.” And he said, “Oh no, no, no. The optimist said ‘We’ll be out by Thanksgiving. No, we’ll be out by Christmas. No, we’ll be out by Easter, we’ll be out by summer.’ And they died of a broken heart.” And so the Stockdale principle is to never confuse your faith that in the end you will prevail with the ability to face the most devastating facts of your current existence.
Pardis Sabeti: And so actually the way we do our work, I’m constantly being like, I believe in what we’re doing, I believe in the outcomes. But right now our sample set is bananas, we have some safety issues… Every day you have to dig in and be like, we’re not being effective, this document is garbage, the safety risks are high. If you’re going to try to work in this space you need to constantly be going under the hood and being really honest with what’s working and not working. When I think about it, every day is a mistake that we’re learning from almost.
Pardis Sabeti: One glorious example is we went on a trip to Nigeria at one point and we were trying to move a set of samples out to be able to ship them back safely to the states. And basically we had PPE on and all of that, but when it released from liquid nitrogen one of the tubes popped in and released gas. And of course then we checked and we looked and that sample was really hot. I was there with two members of my team and we had to basically shut down. The risk was low, it was actually pretty low risk of anything going on.
Pardis Sabeti: And we even called the CDC and all sorts of partners and they said it’s okay. But I remember thinking, they’re like, oh, it’s fine. But obviously don’t get sick while you’re there, because if you do you now have an exposure risk, you’re going to have to be flown back on a jet plane. And all of that was like, oh, wait a second, I actually don’t think we have Lassa, but what’s the probability we’re not going to get sick at some point here and somebody’s not going to eat some bad food or something? And I was like, I can’t take it.
Pardis Sabeti: So basically in that instance we shut the whole thing down and I was like, we got 24 hours to get home. And nobody eat anything until we get there, everybody’s eating the home bars. And basically I get a little crazy. Certainly everyone was like, you don’t need to do this, it’s zero risk. But I made us all go into 21 days of quarantine when we got home, I shuttled everybody to new apartments. I had food going to them, I got MGH and the CDC, I got all these people on board. And it was one of those things where I was like, you know what, that was a mistake and we need to think about it, and that needs to never happen again. And we’re going to do a deep dive and understand why that happened.
Pardis Sabeti: And it was funny because when Ebola came around, MGH was always saying thank goodness we had that simulation, which we essentially did. We simulated what it was like to have to run the possibility of an infection, and it really positioned us very, very well during Ebola to deal with the fact that people were taking real risks of a real outbreak that was spreading. So that was an example. Basically I would say my answer to that question is every mistake is an instructive mistake if you use it the right way. And really I always lean into the mistakes as much as possible, and almost to an annoying fault turn them into an exercise we’re all going to learn from. But when you’re working with deadly viruses that’s not a bad way to be.
Rob Wiblin: Yeah. I think part of the reason why it’s really useful to have this slightly indefatigable optimism that eventually things will work out is just that when we look out into the external world and look at other people’s projects, they look really clean, and like they went to plan, and things are working smoothly and they didn’t cost too much. But then the typical thing when you’re in the thick of a project that’s especially doing something new is that it takes much longer than it seems like it should, and it costs more, and everything is a mess, and stuff’s not working, and the results aren’t as clean or convincing as you hoped they would be. And it’s just that difference between the internal view and then the external PR-facing view gives us a very false impression of what life should be like. And so you have to have this optimism though to overcome the fact that everything seems harder than it should be.
Pardis Sabeti: The other thing I say when I give advice to people is find people you can laugh with. I just remember there was something else that happened on that trip, like right before we left we broke the centrifuge we’d brought out to place there. And I just remember we’re in some airport, I might’ve been like Amsterdam, like halfway through the trip and it’s very quiet. It’s one of those things where the whole airport was… We were on a long escalator, in what could have been a scene from heaven. And we’re sitting there with all of our stuff coming back from this trip, like 24 hours on ground, and we exposed ourselves and broke the centrifuge we brought to place there.
Pardis Sabeti: And I remember just Matt looking at Shervin and I, and he’s like, “Did we tell the lab we broke the centrifuge? And then I just couldn’t stop laughing. Matt was like, “If we were there any longer we would have burned that place to the ground.” And anyway, it was amazing and I think that ultimately there’s a part of it where all of it could be a sitcom. And you have to be with people that you can laugh through it with and you can talk through it with. The fact of the matter is Shervin and Matt are two of the smartest people on the planet.
Pardis Sabeti: And I was the one that actually…that whole situation was my mistake, I made mistakes that led us into that position. And there were no risks in the end, but it was the fact that we even had that kind of a situation was my error. And they are brilliant, and they’re amazing. But the fact that we can laugh and he could just say that, like, we would’ve burned the place to the ground. I mean that’s how you get through it.
Pardis Sabeti: And to be successful you have to be very open about those mistakes, because I think where things get a little dicey is when people get to this place where they have to have a show of perfection. And that’s actually dangerous. Study after study show that when airplanes crash it’s when people are afraid to tell the pilot, “Hey, it doesn’t look like we’re in the right place.” The way you stave off those things happening is having a comfort level, and a humor, and to say when things are wrong. And I think it gets very, very dangerous when we lose humanity and we lose our humor.
Overcoming big challenges [02:10:23]
Rob Wiblin: Yeah. On this topic of overcoming big challenges in life and in your career, you suffered this really horrific car accident in 2015 which almost killed you. And it took days of surgery and I guess years of physical therapy to recover from. I guess it’s the kind of thing you never fully recover from. Most people suffer some horrible setback in their life or career at some point which takes them out of work for months or maybe years. Whether it’s physical illness, mental illness, bereavement, an important project falling apart and breaking their heart. And those tragedies can be really hard to bounce back from. Did you learn anything about how to recover from physical illnesses and personal tragedy from that accident and find a way to get back on your feet?
Pardis Sabeti: Yeah. So just to set the stage, it was actually July 2015 just as things were starting to calm down a little bit after Ebola. And I was at a conference of all places, and basically I was in an accident where I was catapulted onto boulders, and I shattered my pelvis and both my knees. It required I think four all-day surgeries, about 30 hours of surgery. And I now have six plates and 30 giant rods that stitch together my pelvis and my knees. So it’s a lot, it’s a lot. It definitely knocked me into the present, into literally the room I was in and nothing else. I was basically hospital-bound, bed-bound for four months.
Pardis Sabeti: And yeah, it’s a daily recovery process. It’s a lifetime recovery process. And I think the things that I learned from that was that we kind of… In the world today everything seems to be in the mind. And ultimately our mind does not work if our body doesn’t work, it just doesn’t. So the thing is we cannot forget our bodies. It is the engine that runs everything else. And so it forced me to take a moment and say, I need to make this body work. And for somebody who never even takes a day off without doing some work… I couldn’t do anything but that. So I just turned all my attention to doing my physical therapy, becoming a scientist of injury, and trying to figure out how to make my body work. And since then I dedicate a lot of my time, everyday I have to dedicate time to working my body and working all of these scar tissues and bones that are with me as best as I can.
Pardis Sabeti: And so I think that ultimately it’s probably the thing that I learned the most about. If my body is not well then I can’t do my best work, and ultimately you have to support yourself in everything you do. And so I think that also when I run my lab it’s in that same way. I’m constantly trying to, I know I run the team, we run hard. It’s not that we don’t run hard and it’s not that… I mean I pulled more all-nighters than I want to admit this year. But I still always try to hold the fort and say, I have to take care of myself. And so it’s just really important.
Pardis Sabeti: I think the other thing is also how much you can do with exercise and paying attention to it. The fact of the matter is most of these things can be solved. While I love Western medicine, we are way too reliant on it. And I think some of the best support I’ve gotten is from outside modalities that are really remarkable, and I don’t think we use enough other ways of improving our health and our wellbeing. Other than obviously during the surgeries and a few weeks after, I never used any… I stopped using pain medication. Even though it sounds crazy, I found that massage did what I needed to do. Massage is amazing, it’s underutilized. And then after massage, a stretching modality that I use called resistance stretching. Those things were really amazing and are outside of what we call medicine, but I think they were far more potent and powerful. And I think that there’s a lot of really interesting stuff there.
Rob Wiblin: Yeah, I guess it makes complete sense that it’s very hard for the brain to work really well if the rest of the body that it’s attached to isn’t being kept in good shape. Most of my friends take that view, and think that it’s good holistically to exercise, and to stay in shape, and take care of your physical health. Have you found that people don’t think that?
Pardis Sabeti: I think people do that conceptually, but do they really do that? And particularly, like I would say for me, I’ve gone to medical school. Medical school is designed to make you anxious, depressed, and unhealthy. And I always find it really remarkable that basically we would never go to a barber with bad hair or a facialist with bad skin, but our doctors often have such poor health. And so I think for example, it’s pretty remarkable how little personal health is valued in the medical training and profession. And so that’s an example.
Pardis Sabeti: I do think that there are a lot of industries in which personal health is not valued. And it’s sad to me that I think the medical profession has some of the highest rates of suicide and depression of any, and those are the people that are the keepers of our health. So that’s a real issue for me. It speaks to like, what is the integrity of the process you’re doing? And it’s not their fault. You’re just beaten into that. Where it’s all about all nighters and all of that. So I do think that while conceptually yes, people get that that matters, I think in practice, no. Too often not. And I didn’t, I was running myself into the ground.
Rob Wiblin: Yeah, the stories I’ve heard about the indignity and the cruelty that people go through during medical training I found mind boggling. And I mean obviously it’s terrible for them and it’s very dangerous to patients as well, because it means that people can’t do proper work because they’re just being run into the ground. You don’t want your surgeon to be run into the ground.
Rob Wiblin: I’d love to keep talking about this but unfortunately we’ve come up on time, and I know you’ve got a really important grant proposal to work on so I’ll let you go. I guess just one final question is when prepping I heard that you got most of your lab to come stay at your parents house during the Ebola pandemic so that you could all work together and try to get more done. How did that pan out, being in such close contact constantly with your colleagues? Maybe it’s slightly in tension with what we were just saying about the importance of work-life balance.
Pardis Sabeti: I appreciate you did your research. I think the story I’ve told about that was… It wasn’t like we were all working during Ebola at my parents’ house. It was that right before Ebola hit we happened to have been doing a lab retreat at and around my parents’ house. I say it was a Coachella vibe that was teetering on a Fyre festival vibe, where people were in tents and stuff like that, out and about. But we had these very fun activities where we did canoeing and we did sort of team-building stuff, we did a lot of these ropes course-y team-building exercises.
Pardis Sabeti: As it happened, we were actually on our way down to the trip when the Ebola outbreak was declared in Guinea, and two members of my team Kristian Andersen and Stephen Gire had to reschedule and not go on the retreat to go and set up diagnostics in Sierra Leone. And the rest of us went down to this trip. But it was still in Guinea, it wasn’t anywhere where we were. And then we had that and we came back, and we were refreshed, and we were bonded, and we were working together. And then essentially a couple of months later the outbreak was escalating and it came to Sierra Leone and we had to respond in a really big way. And essentially what happened when it came to that is that the Ministry of Health asked us to sequence the samples and find out what was in it, and sequence a whole set of samples and figure out what’s happening.
Pardis Sabeti: So we had to immediately ship the samples back to the U.S., sequence them, put them on… And we had sequenced Ebola before, but never really from clinical samples like this. And so we tried out essentially four different technologies to sequence these samples, and what we did is we paired off in teams and each team took one of the technologies and tried them. And we had to coordinate and we had to have these regular touchpoint meetings. And it was very, very complex, very time-sensitive, and just required a lot of coordination. And I remember thinking goodness, that retreat was really helpful for this. Because there were all of those activities, you’re trying to get across a log and it’s all about just trusting the people you’re working with and communicating with them really effectively.
Pardis Sabeti: And so it was just one of those really terrific things that, yeah, it was serendipity that we just came back and were really high on each other and on working together. And so it was remarkable to see how well we coordinated, how well we tried all the different technologies. When one of them worked everybody jumped over to that one and everything just flew, we were in a flow state. And so it was more about that, it was more just about the fact that building those relationships are so important and it’s not frivolous. It’s actually, it’s core to success. Building those partnerships, and communication, and trust with your colleagues. That was the story.
Rob Wiblin: This has been an incredible pleasure. I hope that in a couple of years time many more people have heard of all these technologies and they’ve really changed the game, and people appreciate what they’re capable of. And maybe I’ll even be able to get one of these things at my doctor’s office in a couple of years’ time.
Pardis Sabeti: Or in your home, yeah.
Rob Wiblin: My guest today has been Pardis Sabeti, thanks so much for coming on the 80,000 Hours Podcast, Pardis.
Pardis Sabeti: Thank you so much for having me, Rob. I really appreciate it.
Rob’s outro [02:20:07]
I hope you enjoyed that interview as much as me!
If you want to work on turning Pardis’ vision into reality, head over to 80000hours.org/advising and learn more about our career advising service to see if it might be able to help you. It’s free of charge and our advisors might be able to point you in the right direction or connect you with people you’d benefit from speaking with.
I also just want to apologize that we haven’t yet nailed the audio quality on all these interviews. We really want to get it right and have been experimenting with new setups, but it’s surprisingly hard to make sure that everything goes right when you’re recording remotely. We’ll keep working on it though, and hopefully will find a reliable solution soon.
The 80,000 Hours Podcast is produced by Keiran Harris.
Audio mastering by Ben Cordell
And as always we’ve got a quality transcript and lots of links to learn more in the blog post associated with this episode, both organized by Sofia Davis-Fogel.
Thanks for joining, talk to you again soon.
Related episodes
About the show
The 80,000 Hours Podcast features unusually in-depth conversations about the world's most pressing problems and how you can use your career to solve them. We invite guests pursuing a wide range of career paths — from academics and activists to entrepreneurs and policymakers — to analyse the case for and against working on different issues and which approaches are best for solving them.
Get in touch with feedback or guest suggestions by emailing [email protected].
What should I listen to first?
We've carefully selected 10 episodes we think it could make sense to listen to first, on a separate podcast feed:
Check out 'Effective Altruism: An Introduction'
Subscribe here, or anywhere you get podcasts:
If you're new, see the podcast homepage for ideas on where to start, or browse our full episode archive.