Emergency episode: Rob & Howie on the menace of COVID-19, and what both governments & individuals might be able to do to help
Emergency episode: Rob & Howie on the menace of COVID-19, and what both governments & individuals might be able to do to help
By Robert Wiblin, Howie Lempel and Keiran Harris · Published March 19th, 2020
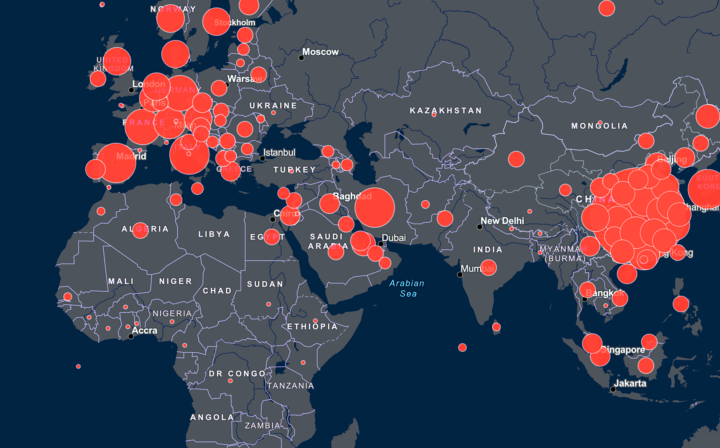
New York Times map of the spread from far back on March 4.
Hours ago from home isolation Rob and Howie recorded an episode on:
- How many could die in the coronavirus crisis, and the risk to your health personally.
- What individuals might be able to do.
- What we suspect governments should do.
- The properties of the SARS-CoV-2 virus, the importance of not contributing to its spread, and how you can reduce your chance of catching it.
- The ways some societies have screwed up, which countries have been doing better than others, how we can avoid this happening again, and why we’re optimistic.
We’ve rushed this episode out, accepting a higher risk of errors, in order to share information as quickly as possible about a very fast-moving situation.
We’ve compiled 70 links below to projects you could get involved with, as well as academic papers and other resources to understand the situation and what’s needed to fix it.
A rough transcript is also available.
Please also see our ‘problem profile’ on global catastrophic biological risks for information on these grave risks and how you can contribute to preventing them.
For more see the COVID-19 landing page on our site. You can also keep up to date by following Rob and 80,000 Hours’ Twitter feeds.
Get this episode by subscribing to our podcast on the world’s most pressing problems and how to solve them: type 80,000 Hours into your podcasting app.
Producer: Keiran Harris.
Articles, books, and other media discussed in the show
Academic resources
- The famous Imperial College London study comparing mitigation and suppression: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand by Ferguson et al. (16 March)
- Critical review of that paper “Impact of non-pharmaceutical interventions…” by Shen et al. (March 17)
- Reasons why suppression may struggle to work: Analysis of 25,000 Lab-Confirmed COVID-19 Cases in Wuhan: Epidemiological Characteristics and Non-Pharmaceutical Intervention Effects, by Xihong Lin. And Rob lists scenarios under which the UK might need to switch away from its current plan.
- Argument that suppression or containment might be too costly to be worth pursuing: Has the coronavirus panic cost us at least 10 million lives already? by Paul Frijters
- Lessons from containment efforts in Singapore by Lee et al. (13 March)
- Possible Fiscal Policies for Rare, Unanticipated, and Severe Viral Outbreaks from Bill Dupor at the St Louis Fed (March 17) and a breezier set of economic policy suggestions from Greg Mankiw (March 13)
- Response to COVID-19 in Taiwan Big Data Analytics, New Technology, and Proactive Testing by Wang et al. (March 3)
- Adjusted age-specific case fatality ratio during the COVID-19 epidemic in Hubei, China, January and February 2020 by Riou et al. (March 6)
- Clinical data on 1,099 patients hospitalized in China before January 29, 2020: Clinical Characteristics of Coronavirus Disease 2019 in China by Guan et. al. (Feb 28)
- Basic descriptive analysis of 72,000 patient records reported in China through Feb 11, 2020: Vital Surveillances: The Epidemiological Characteristics of an Outbreak in China CDC Weekly
- A Single Ventilator for Multiple Simulated Patients to Meet Disaster Surge by Neyman and Irvan (2006)
Approaches of specific countries
- Why Singapore’s coronavirus response worked – and what we can all learn by Dale Fisher on The Conversation (March 18)
- Which Country Has Flattened the Curve for the Coronavirus? in the New York Times (March 19)
- Without serious action, Australia will run out of intensive care beds between 7 and 9 April by Megan Higgie and Andrew Kahn (March 18)
- How crowded Asian cities tackled an epidemic by Hannah Beech for the New York Times (March 17)
- Korea’s Drive-Through Testing Is Fast — And Free by Anthony Kuhn for NPR (March 13)
- The FDA/CDC coronavirus response is one of the most shocking government failures I have seen in my lifetime by Alex Tabarrok (March 9)
- Website tracking each country’s COVID-19 policy response
Dashboards, models, figures and data analysis
- The best coronavirus dashboard: live updates, cases, death toll, graphs, maps, and compare countries
- Coronavirus Statistics and Research from Max Roser, Hannah Ritchie and Esteban Ortiz-Ospina at Our World In Data
- How many tests are being performed around the world? from Esteban Ortiz-Ospina at Our World in Data
- Epidemic calculator for rough scenario modelling
- Modelling for policymakers: Why you must act now
- Data mapping from JHU GSSE. You can do your own analysis using the source CSVs.
- Great website offering coronavirus projections and comparing cases and deaths to ICU bed numbers made by Chris Billington
- Stay abreast of new developments by reading coronavirus articles at the Financial Times
- A page listing even more COVID-19 dashboards
Projects being undertaken by individuals and groups
- Help with COVID — A compilation of COVID-19 projects looking for volunteers
- Project Open Air — A group working on medical devices, to have a fast and easy solution that can be reproduced and assembled locally worldwide
- Pledge to #StandAgainstCorona – Four important steps can help slow the spread of COVID-19.
- Coronavirus Tech Handbook compiled by Nathan Young
- Crowd Fight COVID-19 appeal for volunteers
- Promoting simple do-it-yourself masks: an urgent intervention for COVID-19 mitigation, by Matthias Samwald and co-authors
- Looking at South Korea’s amazing progress through Rob’s scrappy projection models
- Coronavirus: Tens of thousands of retired medics asked to return to NHS, covered in the BBC
- GM’s CEO Offers to Make Ventilators in WWII-Style Mobilization by Jordan Fabian and David Welch in Bloomberg
- COVID-19 Open Research Dataset from Semantic Scholar
- Offering Funding for COVID-19 Projects by Sam Altman
- COVID-19 Testing Charts by Spencer Chen
- Prepare Now for the Long War Against Covid-19: Fighting the surprise attack should not distract us from the lasting battle by Richard Danzig & Marc Lipsitch in Bloomberg (March 20)
- A hospital begins UV sterilizing masks for reuse
Highly simplified explanations for rapid understanding
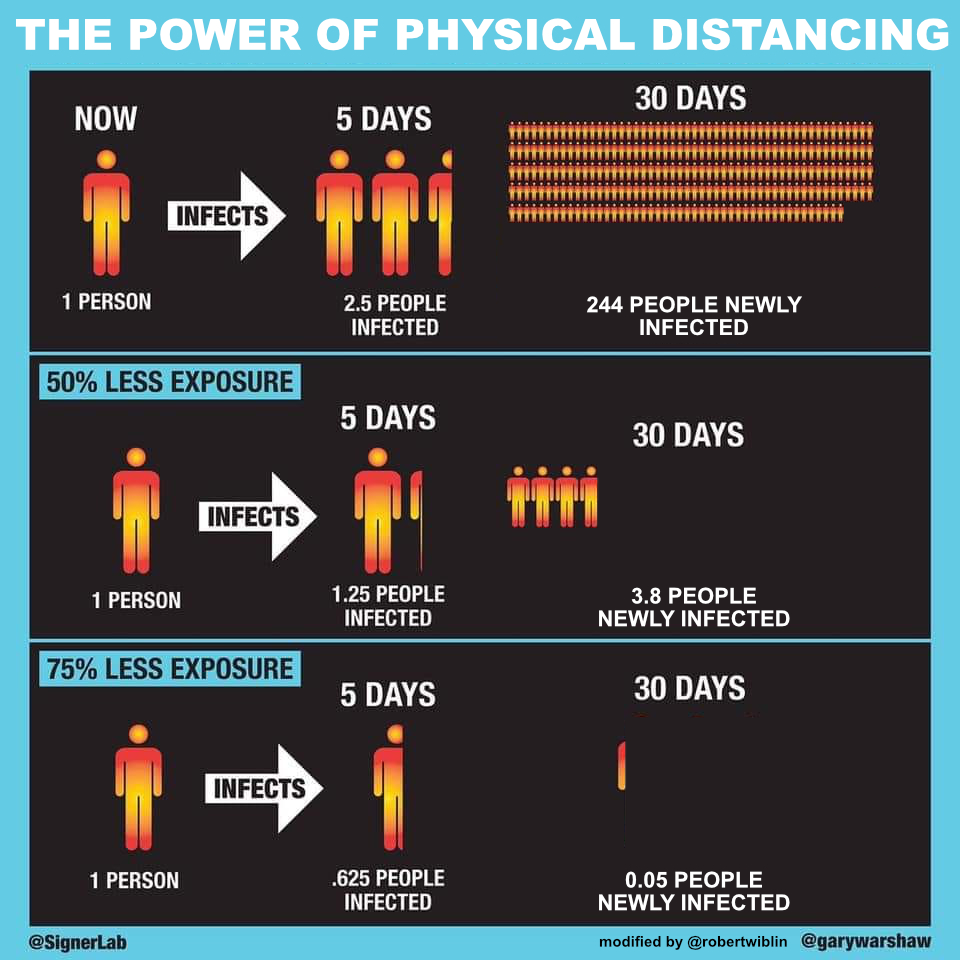
- How to explain the unexpectedly large impact of physical distancing, especially to your less mathy friends and family
- The UK Government’s current strategy to combating COVID-19 in very brief form, and the case in its favour: one, two, three, four
- Viral video that shows you how germs spread
Pharmaceutical and medical interventions
- Handbook of Covid-19 Prevention and Treatment from Hospital with 0% fatality from the Zhejiang University School of Medicine
- Translation of the Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia from the Chinese Health Commission (March 3)
- A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19 by Cortegiani et al. (March 10)
- Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro by Liu et al. (March 18)
- Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro by Wang et al. (February 4)
Figures
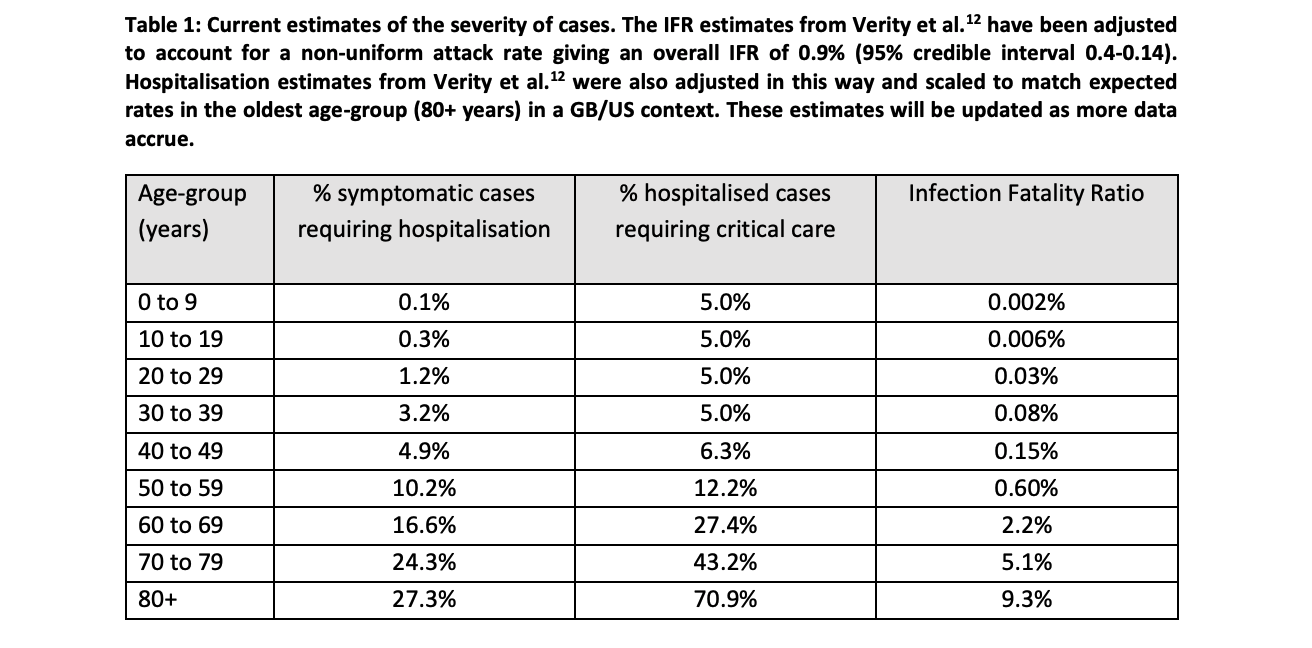
One: Estimates of fatality and hospitalisation rates by age
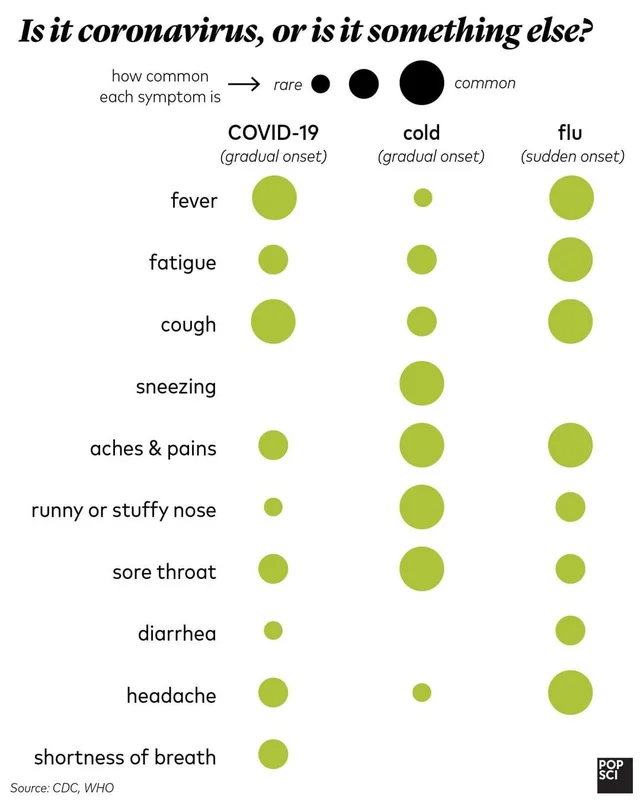
Two: Do you have COVID, or is it more likely something else?
Note: In the time since this graphic was created, we’ve heard preliminary reports that diarrhea and other gastrointestinal issues may be the primary early symptoms for a moderate number of patients.
Three: A simple visualisation of exponential growth
Other news stories lifted from Hacker News that may be useful
- Ten-Minute Coronavirus Test for $1 Could Be Game Changer by Alonso Soto (March 16)
- Government official: Coronavirus vaccine trial starts Monday by Zeke Miller (March 15)
- Italian hospital saves Covid-19 patients lives by 3D printing valves for reanimation devices by Davide Sher (March 14)
- Up to 50% – 75% of cases of Covid-19 could be asymptomatic (March 16)
- COVID-19 Has Caused A Shortage Of Face Masks. But They’re Surprisingly Hard To Make by Emily Feng and Amy Cheng (March 16)
- Is It Time to Rethink Globalized Supply Chains? by Willy Shih in the MIT Sloan Management Review (March 19)
- Alphabet, Walmart join U.S. effort to speed up coronavirus testing (March 16)
- FDA grants Roche coronavirus test emergency green light within 24 hours by Conor Hale (March 13)
- Nvidia calling gaming PC owners to put their systems to work fighting Covid-19 by Connor Sheridan (March 13)
- Face Mask Use and Control of Respiratory Virus Transmission in Households from CDC
Wikipedia on country outbreaks
- The 2020 Coronavirus Pandemic in: New Zealand, South Korea, Australia, United Kingdom, Italy, Spain, France, the United States, Taiwan, Singapore, Japan, Iran.
Government resources
- Relevant publications from the UK’s Scientific Advisory Group for Emergencies (SAGE)
- UK guidance for households with possible coronavirus infections
- Hygiene promotion poster from Singapore: Let’s all do our part
See also this list of resources from the folks at LessWrong.
Transcript
Table of Contents
Rob’s intro [00:00:00]
Robert Wiblin: Hi everyone, as you might expect under the circumstances, today’s episode is our second impromptu recording about the COVID-19 crisis.
Three quick notes first. In this episode we spend a fair while at the start laying out the general situation that faces us — including where the virus is, in what numbers, how many have died and where, the properties of the virus and the disease and so on.
If, like many people, you’ve been obsessing about this for the last few days or weeks or possibly months, you may feel fine to just skip that section and jump to minute 31 after which we talk about things you’re less likely to know about. If your podcasting software supports chapters, we list 5 of them in this episode.
Second, if you’d like to follow along with my non-80,000 Hours-checked personal opinions as I’m learning about COVID-19 you can please follow me on Twitter at twitter.com/robertwiblin.
Third, we are going to have more articles about COVID-19 which you’ll be able to see when they go on up at 80000hours.org / blog. We’ll also post that as well as other work and articles that we think are interesting at twitter.com/80000hours.
OK, stay safe out there everyone. Here’s me and Howie.
The interview begins [00:01:08]
Robert Wiblin: All right, so we’re here, me, Robert Wiblin and my colleague, Howie Lempel, for what is very much an emergency edition of the 80,000 Hours Podcast to talk about the spread of COVID-19, what the situation is, and what potentially people can do about it, both individuals and governments. How are you doing, Howie?
Howie Lempel: I’m doing well. Happy to be here.
Robert Wiblin: Yeah, I guess I could be happier to be here. I’m actually out in the country. I left London a week ago. But Howie, you’re camped out in your house in London?
Howie Lempel: Yes, I am camped out and isolating myself at the moment.
Robert Wiblin: Because you have cold symptoms, right?
Howie Lempel: Yes. I started getting cold symptoms. Seemed pretty minor, but we figured be as cautious as humanly possible. And so our housemates went out and got an Airbnb to avoid us and now my girlfriend and I have the house to ourselves as we wait to make sure that neither of us are actually sick.
Robert Wiblin: Yeah. We apologize if the audio here is not so good. We didn’t manage to get all of our equipment out of the office and into the different places that people on the team are in time. So this is a slightly more scrappy episode than usual and perhaps even scrappier than our last COVID episode that we did. All right. Well maybe we should start by talking about our qualifications just so people can have some sense of how seriously to take what we’re saying. I guess as many listeners will know, my background is in economics. I also did a science degree. I guess my main qualification to talk about this is, I’ve been paying attention to the COVID situation for two months and I guess the last two or three weeks living, breathing, eating COVID-19 stuff basically all the time. And I guess particularly the last week, I’ve more or less done nothing else. Yeah, Howie, I guess you actually have more of a background in the area than me.
Howie Lempel: Yeah, so my academic background was largely in math and economics and then a little bit of moral philosophy. And then I spent a couple of years in law school in the US and then left to go work for Open Philanthropy where I spent a few years. And when I was at Open Phil, I helped to get our biosecurity and pandemic preparedness program areas started up. We then later handed it off to somebody who is actually an expert, so I should be very clear that I myself am not one. I don’t have any formal training in any of the related areas, but hopefully I picked up something or other in the experience of searching for an expert, making our first couple of grants, trying to learn the space.
Laying out the current situation [00:03:57]
Robert Wiblin: Yeah. I’ve gotten a little bit more confident about trusting our judgment in the last few weeks because it seems like things have played out much more closely to what we expected in late January and early February perhaps than what many other people were predicting. Because we had a view that there was a good chance that this could just spread everywhere and get out of control and be a worldwide pandemic, that it could kill something in the order of 1% of the world’s population, that that was plausible. We made, I guess, estimates in those early days about the case fatality rate, the infection fatality rate, the transmissibility, that now all seem kind of consistent with what we’ve seen over the last six weeks.
Howie Lempel: Yeah. I haven’t gone back and re-listened, but that all sounds just about right to me. I guess the thing that feels most surprising to me, relative to what I believed then, is how good of a job China has done of containing the disease in mainland China. I think that that was something that I hadn’t expected with a respiratory disease that a country so big would actually be able to shut down an outbreak that had already spread so far.
Robert Wiblin: Yes, that was quite surprising to me. And I guess initially when they started reporting such a trail off in new cases, I was suspicious that this could be a measurement error somehow. I think we did say at the time that it was just we were in uncharted waters in terms of the severity of the shutdown that China was doing. That basically no one else had done this before. So we just didn’t know what the effect of it was going to be, but it was more than what I thought. Basically, it seems like China, to a large extent, has control of the pandemic for now, and the question is, will they be able to maintain that while returning to something resembling normal life?
Howie Lempel: Yeah, that seems right.
Robert Wiblin: All right, let’s move on and just give people a sense of the state of play. As of, I guess we’re recording at, you have to say the time of day these days, recording at 16:30 in London on the 19th of March. And as of now, we’ve got about 225,000 confirmed cases globally. But in reality, we would guess that at least there’s 10x that number of actual people infected worldwide, potentially quite a bit more than that. About half that number is in China, where we now think that the pandemic is largely controlled as we said. So most of the growth is occurring outside of China and we’re getting about 15 to 20,000 new confirmed cases a day with a special concentration in Europe in particular; I guess France and Spain. Sorry, Italy is actually at the top. Some in Switzerland and Germany and the UK. But they’re reporting particularly large increases. And we’re seeing, I guess, about a 15 or 20% increase day-on-day of out-of-China cases. Is there anything you want to add to that, Howie?
Howie Lempel: Did we also catch Iran?
Robert Wiblin: Oh, sorry.
Howie Lempel: Which is another country that has a really high caseload.
Robert Wiblin: Yeah, sorry. It seems like there’s an enormous number of cases in Iran, but I think their testing capacity is lower, so it shows up less if you just look at the confirmed case increase or at least it did when I last checked, if I recall.
Howie Lempel: Well, I guess it has the third most total confirmed cases after China and Italy, so it’s up there.
Robert Wiblin: So it’s up there. Nice. Okay. Yeah. Just checking on Iran, they’ve got 18,400 confirmed cases, 1,300 deaths or so. And I guess in the last day they reported, let’s see, about a thousand new cases, which is a 7.3% increase. Yeah, it looks like the case increases have been linear for quite some time, which I suspect is because of bottlenecks in testing rather than the cases actually growing at a linear pace. Anyway, yeah, globally we’ve got about 9,300 people reported dead, which would give us a case fatality rate around 4%. At least that’s what the figure was yesterday.
Howie Lempel: Going quickly back to the data in China, it looks like now just about a third of current cases or of total confirmed cases are in China. I think that there’s this perception that this is sort of like a Chinese virus, a Chinese disease, that sort of started to affect everybody else. And it seems worth noting that that’s just not the case anymore and that most of the confirmed cases at this point are happening outside mainland China.
Robert Wiblin: Yeah, at this point, China should be stopping anyone from coming in rather than the reverse. They have a lower density of cases than many other places. Yeah. Okay. In terms of deaths, we’ve got, I think, put these numbers in yesterday, 9,300 deaths globally, which was about a 4% case fatality rate based on the number of confirmed cases at the time. Keeping in mind, of course, many people were confirmed recently so they won’t have passed away yet. And at the same time, we think we’re only capturing a small fraction of all of the cases that are actually out there. So that kind of raw case fatality rate doesn’t tell you all that much.
Robert Wiblin: But we can see interesting variation between countries. In South Korea, they’ve had 8,400 confirmed cases and done the most stringent testing regime of anywhere outside the Bhutani Gulf States. And they had a case fatality rate of 1%, so they’ve had 84 deaths out of 8,400 cases. By contrast, in Italy, they’ve had about 36,000 confirmed cases and almost 3000 deaths, which just translates to about an 8.3% case fatality rate. So an eightfold difference there, which I think is partly probably due to the different demographic breakdown that Italy is an older country. But also I think it suggests that we’re capturing a far smaller fraction of all the infections as confirmed cases in Italy. And you see that in the different confirmation rates within the testing. So in Korea, they’ve got, I think a 3% confirmation rate on tests while in Italy, when I checked yesterday, it was more like 20-21% which was among the highest in the world, which suggests that there’s a vast number of cases in Italy that are not being tested for. And if they were able to test more people, they’d find that there is way more people who have it than what is measured.
Howie Lempel: Yep. And in those cases, usually the people who do get tested are the people with the most severe cases. That’s a second mechanism for why you end up overestimating the case fatality rate.
Robert Wiblin: Right. So last time I think we pointed to some piece of research that suggested that the best estimate of the infection fatality rate, that is, the probability of someone dying if they actually get infected rather than if they’re confirmed through some test to be infected was about 1%. Where are we on that research now, Howie?
Howie Lempel: Yeah, I think the best answer is that it hasn’t changed all that much. It’s more complicated now because there are more estimates out there and people are now trying to do estimates that are sensitive to the differences between places because we don’t expect the infection fatality rate to be the same in every country depending on their medical system, depending on what interventions they choose. But a couple of recent estimates were 1), coming from a top modeling group at Imperial who used a 0.9% overall infection fatality rate as their assumption for what the infection fatality rate would be in Great Britain if Great Britain didn’t take any more measures than it currently is. So that’s sort of like a world where the hospitals really do fill up and get overwhelmed. And then another estimate that I thought was particularly good based mostly on data in China found a 1.6% overall infection fatality rate. So I think you’re going to see most of the estimates somewhere in that 0.8 to 1.6% range if you’re talking about basically situations that look fairly similar to the situations that we’ve seen so far.
Robert Wiblin: Okay. So that infection fatality rate is going to vary a bunch based on whether the hospital system is overwhelmed which is a big concern that people have. Do you have any sense of what the range would be between getting it early when the medical system is functioning well to getting it during a peak when most people are going to struggle to get medical attention?
Howie Lempel: Yeah, I think it’s really hard to say. So the big constraints that we know of are going to be the number of ventilators that they can use. Basically, if your lungs stop working, they can mechanically sort of breathe air into you in ICUs. And so that’s a life saving procedure. And then the people to operate those ventilators. And our best guess right now is that those are sort of the two main constraints. It doesn’t seem like almost any country is going to have the capacity to treat everybody who needs access to these ventilators if the pandemic is just allowed to sort of go forward without any major interventions.
Howie Lempel: And so a question is, well, how high exactly the case fatality rate are we talking about if we don’t do that? And it’s really hard to estimate because you might want to compare to the data we have from China where they had an infection fatality rate of about 1.6%. But we don’t exactly know how much access to this equipment those patients had. So I think best guess is that moderately crowded hospitals are going to lead to infection fatality rates in the 1 to 1.6% range. And then as they get much more overwhelmed, you’re going to sort of see them higher than that. And if you can get them less overwhelmed, you’re going to see them go down. So that’s my sort of really high level take on it.
Robert Wiblin: Yeah, so that sounds about right. I guess in Hubei, even though there was a ton of cases, they benefited from the fact that they could send medical staff and equipment from the rest of China, which I guess meant that things were kind of in an emergency situation but not completely overwhelmed necessarily and they were famously building those hospitals incredibly quickly. But if it was allowed to just overrun entire countries or entire continents, then everyone would just be in the same impossible situation.
Howie Lempel: Yeah. I don’t have a sense like just quantitatively how much exactly, and at what point the help from other provinces ended up making a big difference in Hubei.
Robert Wiblin: I don’t know either. You were saying if it spreads uncontrolled, then not everyone will be able to get that equipment. It seems like if it’s spread uncontrolled, approximately nobody who needed equipment, like roughly 0%, would be able to get medical assistance, which I guess is why this seems like it’s just such an incredible emergency potentially. Like the biggest global emergency that we might live through, potentially. That something has to be done to stop this progress. Otherwise, we could see fatality rates above 1% of the whole population.
Howie Lempel: Yeah, that seems right. And I guess when we’re talking about running out of ventilators, I think it’s often easy to slip into thinking about rich countries and the fact that they do have some spare ventilator capacity. And you can imagine them scaling it up and then there’s a whole bunch of countries that are going to have even less capacity than the places that most of the models are coming from. So should be even more worried there.
Robert Wiblin: Yeah, it’s interesting. We might get to talking about those countries later in this episode, or might have to save it for another episode, because I haven’t done enough background research to understand what the situation is in India. I guess one thing that those countries have going for them is sometimes that it’s quite a bit hotter, which apparently can make it harder for the virus to spread. But I guess we also just have incredibly poor data in many of these countries to indicate what is the level of penetration of the virus at this point.
Howie Lempel: That’s right.
Robert Wiblin: Okay. So yeah, severity of the illness. What fraction of people are asymptomatic? What fraction of people will have a serious flu, and what fraction of people is it life-threatening for?
Howie Lempel: Yeah. So I think we don’t yet have excellent data on any of this, but I can give you a sense of what’s out there. So on what percent of patients are asymptomatic, one of the best measures that we have is we can look at data from the Diamond Princess, which was this cruise ship that had a terrible outbreak. And a very high percent of the people on the cruise ship ended up getting tested. So they got tested even if they were asymptomatic. And we can then look at, okay, out of all the people who are infected, how many of them were asymptomatic. And depending on how you measure, I think you end up getting something like 45% to 55%. The issue there is that it has a fairly long incubation period. So from when you get infected until you start getting sick, even if you’re eventually going to be symptomatic, there’s going to be a long period of time. So we don’t know how many of these asymptomatic people from the Diamond Princess, once they left the ship, ended up developing symptoms. So you can sort of think of that number as like an upper bound.
Robert Wiblin: Yeah, there’s also some more recent report of, I think, 3000 or so people who were tested in an Italian village where they found about 50 to 75% they estimated were asymptomatic currently. But that’s suffers maybe even more severely from this issue that many of them will develop symptoms in future. And it’s very frustrating that more followup wasn’t done on all of the people from Diamond Princess. It seems like a massive oversight because we could have gotten a much higher quality dataset there.
Howie Lempel: Yeah, I’ve actually been looking into this and it seems possible there’s some data out there. Worldometer seems to have some follow up, but it’s just entirely unclear where it comes from. So I don’t know how thorough it will be or anything like that.
Robert Wiblin: Yeah, I like Worldometer as a website and it is incredibly frustrating how poorly they source their data. Usually when I’ve looked into it, it is real. They’re not just making stuff up. But you have to hunt around for where they’re getting it from.
Howie Lempel: Yeah.
Robert Wiblin: Okay. So that’s the asymptomatic cases. How about the severity breakdown?
Howie Lempel: Yeah, so the heuristic that people have been using has been something like 20% of cases are severe.
[Ed: After this episode was released, we learned that some prominent studies use a weaker definition of ‘severe.’ Our heuristic is now to think of ‘mild’ as everything from asymptomatic through ‘flu/pneumonia that’s at the borderline of requiring hospitalization.’
We’re generally thinking of severe as ‘flu/pneumonia that requires hospitalization and oxygen’ to ‘in need of mechanical ventilation in an ICU.’
Definitions vary across studies, though, so it remains important to track exactly what definition is being used.]
Howie Lempel: And severe means, in my opinion, like actually quite severe. And it depends by the study, but usually it’s defined as something like needing to go to an ICU because you’d need a ventilator to assist your lungs. That’s a pretty serious situation. A bunch of people who end up in that situation don’t end up making it. There’s some chance that you’ll end up with longer term damage from going through that. But it is good that it’s only about 20% of people as far as we know. And then the other 80%, if that’s right, would be a combination of people who are seriously ill, who maybe have pneumonia but pneumonia that’s not bad enough to get them put into an ICU to people who have flu-like symptoms to people who are nearly asymptomatic or asymptomatic. And so that’s sort of the range of severity. And I don’t think we have a lot of precision within that about exactly how it breaks down between those categories.
Robert Wiblin: Yeah, so this might be a good time to talk about this table that we found in this muddling from Neil Ferguson’s group at Imperial College London, which has had a big influence on the conversation over the last few days. In table one, they have infection fatality rate estimates by age, from Verity et al., a paper that I have not looked at, at all. And so they try to estimate using the percentage of symptomatic cases that would require hospitalization, which I guess gives you a sense of the fraction there that are critical. And then they also try to break down the percentage of hospitalized cases that require critical care, which I guess, in this case, is something like a ventilator and potentially a full staff member to monitor them.
Robert Wiblin: So for people in our age group, which is thirties, which is what I looked at first perhaps unsurprisingly, they had a 3.2% requiring hospitalization estimate. Five percent of those would require critical care, and then they had an infection fatality ratio estimate of 0.08%, so about one in a thousand. Interestingly, as you go below that, all of those rates decrease a lot. Even for young children, it seems like the disease is affecting young children much less than even middle-aged people to the point where it seems like it’s very rare for someone under 10 to die. I guess possibly newborns could be affected worse. But people under 30 don’t need to worry so much for themselves. They mostly need to worry about the fact that they’re going to infect and kill other people.
Robert Wiblin: These numbers ramp up a lot for people who are older though. So if you’re 40 to 50, then you’ve got a 5% chance of requiring hospitalization. 50 to 60 it’s more like 10%. 60 to 70 it’s 17%. 70 to 80 it’s 24%. And then 80 plus, they estimate 27%. And similarly, the infection fatality ratios that they estimate go from 0.1% for you and me Howie, to 0.15% for people in their forties. 0.6% for people in their 50s. 2.2% for people in their sixties. 5.1% for people in the 70s and all the way up to 9.3% fatality rate for people in their 80s. So very severe numbers potentially for people who are older than us.
Howie Lempel: And do we have a sense of why the numbers are differing so much by age?
Robert Wiblin: Interesting. Yeah, I don’t know off the top of my head. I guess in general it seems like the flu affects people who are older potentially a lot worse, but I’m not sure exactly why that is either.
Howie Lempel: Yeah. I guess one theory is that it actually is specifically to do with age and I think that’s certainly playing a role. I think lung capacity gets a bit worse as you age. Another big proportion of it I think is that people with pre-existing conditions have done a bunch worse.
Robert Wiblin: Yeah.
Howie Lempel: And older people are much more likely to have additional health issues. So that might give some sense that a particularly healthy person in one of the older age groups might expect outcomes that look a bit different from the ones here.
Robert Wiblin: Yeah. Unfortunately, I still have not seen a multivariate regression or a cross tabulation of the fatality rate by both age and pre-existing conditions, which would be extremely helpful to have because let’s say that you’re in your 70s, but you have no heart problems, no lung problems, no other health conditions. It could be that your infection fatality rate could be quite low, but unfortunately no one has yet done that analysis, at least, I haven’t seen it yet.
Howie Lempel: And then I guess a really scary other option for why the infection fatality rates get so high for people who are older. So we’ve started to hear some really scary reports about the triage decisions that doctors are having to make. And one of the main ways that they make those when there aren’t enough ventilators for the number of people who need them, sort of look at expected healthy life years going forward. And so it may be the case that young people are just getting first access to the ventilators that everybody needs to stay alive.
Robert Wiblin: Yeah. I guess there’d be two things there that they might considering. One is, the number of years of healthy life that they have left, but also their chances of surviving. That potentially if the chances of someone making it just drops too low, then they decide that they have to prioritize someone else who has a better shot.
Howie Lempel: Yep.
Robert Wiblin: Okay. So what do we know about how it’s caught? Do we know more than we did a month and a half ago?
Howie Lempel: My sense is that we don’t know more than we did a month and a half ago. So I think what we know is that the virus will stay on certain surfaces like steel for up to three days, although it degrades over that period of three days. At the end of three days, it’s going to be very little left.
A recent study showed that the virus could remain viable in the air for several hours when a mechanical device was used to keep it suspended as an aerosol. In contrast to what we suggest in the episode, the study did not show that the virus could remain suspended in the air on its own.
Howie Lempel: It seems like it hangs in the air in an ideal laboratory condition up to like a few hours, although even there it degrades really quickly. And then we can take that and then we can take what’s known about how people have gotten sick, who their contacts have been, and sort of make some guesses. So the best guess that we have is that most of the transmissions are happening through a couple of mechanisms.
Howie Lempel: One of them is through droplets. That’s when someone coughs and the droplets that come out directly land on someone else. Another mechanism that seems likely to be playing a big role is fomites. And so that’s when someone gets some virus particles. Maybe they cough into their hand and then they touch something. Now there’s just virus particles lying on that thing. Then someone else comes by, touches it, now they have virus particles in their hand. They touch their face and they get infected. So that seems like another potentially major mechanism. And then there’s direct contact. And so that basically means that if you shake hands with somebody who is sick and it’s reasonably likely that they touched their face fairly recently, it’s reasonably likely that you’re going to touch your face after it happens. And so the virus sort of gets transferred and you get sick that way.
Howie Lempel: So those are the ones that we have the strongest consensus on. Other possibilities, one of them is fecal-to-oral transmission. There’s some evidence that some of that is happening. So that can happen, for example, if you’re in a public bathroom: you flush the toilet and if the seat’s not closed, that flush can sort of throw a whole bunch of microscopic aerosol particles up into the air. And if some of those are dangerous, you’re exposing yourself to those.
Howie Lempel: And then another possibility is that some of it is going through aerosol transmission, which is when someone coughs or even maybe when someone spits or breathes, they sort of expel out even small droplets of water that are able to hang in the air for a while. And those can sort of travel farther and lasts longer. And so when you hear about staying six feet away from people, part of what’s going on there is it’s sort of a guess at how far those aerosols might go, in case the aerosols are driving some of the infection. I haven’t seen any strong evidence, but the thing that everybody seems to believe, which is very unlikely to be the case, is that the virus is actually airborne in a sense that virus particles themselves just stick in the air and stay there for hours to days and can fly more than six feet. So as far as we know right now, there’s no reason to think that.
Robert Wiblin: Yeah. How controversial is it that just merely breathing and then someone being six feet away, or I guess less than six feet away, that you can catch it that way without someone coughing? Do many people think that’s definitely the case?
Howie Lempel: This feels like I’m a bit outside of my area of knowledge. My read on what I’ve heard from the virologists, epidemiologists and doctors I follow on Twitter is that people mostly say they don’t think that just being breathed on is where most of the transmission is happening. But it’s also just absolutely possible that some virus is being expelled when that happens. And I think nobody would be shocked to learn that some substantial amount of transmission turned out to be happening that way, is my read of the situation.
Robert Wiblin: Yeah. Okay. It seems like there’s been a lot of messaging around washing hands and not touching surfaces. And I wonder why there hasn’t been more of a focus on covering up people coughing, because I think there’s good reasons to think that in public spaces, where people are moderately crowded or even in say a supermarket, someone coughs and then those droplets hang around for a while and then just people around you could pick up the illness. I suppose maybe it’s somewhat harder to deal with and in the West we don’t have as much of a culture of wearing face masks that might help to protect against that. But I guess I would like to see more work on that because I expect people have already picked up the hand washing message quite a bit.
Howie Lempel: Yeah, I don’t know why it’s been less of a message. I guess part of it is it might be just harder to build the habit. So it comes out of nowhere. Part of it might be that actually sneezing into your elbow still doesn’t block all of it and maybe it’s only somewhat effective. Yeah, but I guess I’m not entirely sure why that is.
Robert Wiblin: Okay. So the incubation period we think is what, two to 14 days with a handful of outlier, unusual cases. But typically people develop symptoms three to five days after being exposed to the virus. Is there anything to add on that?
Howie Lempel: No. I think people should have five days as the average in their head, and they should think that after 14 days it’s quite unlikely that someone develops it.
Robert Wiblin: Yeah. And how long do people stay sick for?
Howie Lempel: We’ve seen lots of data on this and it differs by the sample you’re working with. But if you had in the back of your mind about two weeks if your case is not severe. So basically if you don’t end up needing to be hospitalized, or need to be hospitalized, but it’s fairly minor in that category. If you’re thinking two weeks around, don’t be surprised if it’s a bit longer than that. And then severe, I think, can last somewhere between three weeks and six weeks.
Robert Wiblin: Yeah. I’ve seen figures suggesting that people who need intubation or people who need medical assistance to help them breathing could potentially require that for several weeks at a time, which was more than I was thinking. And suggest that they’re going to have potentially symptoms for a long period of time as they try to recover.
Howie Lempel: That’s right.
The importance of isolating yourself [00:30:32]
Robert Wiblin: Okay. That’s the scene set. Let’s move on to think about what we think people should be doing or at least the basics of what people should be doing which, in my view, in most places right now, certainly most places our listeners are, is self isolation to stop transmission. Basically, I’m a supporter of everyone who can stay at home, without society collapsing in their absence, should be staying at home. That means no eating out, no going to clubs, no socializing in large groups, no parties. The things that seem least harmful if you need to get out or not be alone is walking alone either outside or in one-on-one situation in a non crowded area or meeting someone one-on-one in your house without having contact with others. Those create much less of a risk of transmission than people being in crowds. Is there much more to add on that, Howie?
Howie Lempel: Yeah, I guess I agree with everything Rob said and then just sort of want to acknowledge the reality that self-isolation is just not a possibility for lots of people. People who have to go to work, people who are doing critical jobs. And so I guess isolation makes it sound like a binary. And what we actually most care about is physical distancing than social distancing. So you know, to the extent that you can create fewer close contacts between you and other people by taking any of these steps, you’re reducing the likelihood that you get sick. You’re reducing the likelihood that if you get sick, you pass it on to others.
Robert Wiblin: Yeah. Fortunately it looks like government policy is coming along to provide income support to people or relief on their rent or on their mortgage payments or bills so that people can potentially stop working even if they are not in a salaried job where they might continue to be paid anyway. And I think that that is something that we do desperately need. That everyone who can stay home and everyone who society can kind of pay to stay home should be doing that at this point. At least in countries where we know that the virus has reached in any significant numbers. You’re exactly right. It’s about physical distancing, not social distancing. So if you can talk to people on Skype, get on the phone, hang out with people that way, then that’s completely fine.
Robert Wiblin: It might be worth us explaining why we think it is important for people to take what might seem like a drastic step to them if they haven’t been following this for several weeks. And I guess that’s just that if each person who has this transfers it to 2.5 other people, then it’s just going to explode. The case numbers are going to explode exponentially. And the hospital system is going to be completely overwhelmed.
Robert Wiblin: If we managed to cut down the number of contacts that people have by 50% or 75% by getting them to mostly just stay in their house and socialize with no one or just with the same few people repeatedly, then rather than have the case numbers explode, we can actually have new cases decrease as we’ve seen in some countries. Potentially we can have the virus go into recession in a sense and then we can begin to loosen up those restrictions and return to normal life hopefully without the virus then coming back and creating an enormous peak in cases that would just overwhelm the hospital system and society as a whole. Anything to add on that, Howie?
Howie Lempel: No, that seems right to me.
Robert Wiblin: Yeah. So there’s this interesting phenomenon that you may not know many people who have caught COVID. You may not know anyone who’s died of it yet. But we have to implement these quite stringent physical distancing measures before that happens. If we only implement them at the point when you’re likely to know someone who has it or even someone who’s died of it, then it will be far too late. And we would have to engage in this physical distancing for a very long period of time. Or it could just be that it’s too late for that to function, to stop the virus from spreading to a vast number of people. It’s just the nature of exponential growth that things are picking up so fast that the only way to maintain control is to do it while you know one in a thousand or ideally fewer people have caught the virus yet.
Robert Wiblin: Okay. So some other advice that we might be able to offer that is fairly straightforward is that if you start getting symptoms of illness, you need to rest up. And it’s much more important than usual for two reasons. One is let’s say that you are getting a cold or the flu. This is a really bad time to be getting that for your own health because it’s possible that you will then catch this other much more serious virus later and you ideally don’t want to have two respiratory illnesses simultaneously. So you want to get over this initial thing, if it’s not COVID, as quickly as possible.
Robert Wiblin: Secondly, if you do have COVID, there’s a risk that it could become serious. If you say just keep working or you don’t rest sufficiently to cure it or to clear the virus without having serious symptoms, then you could end up needing to go to hospital, end up needing medical attention and in the current environment if they’re treating you, they may well not be treating someone else so you’re potentially imposing a huge burden on someone else who then won’t be able to get a respirator or won’t be able to get medical attention because you didn’t stay in bed. Because you didn’t take care of yourself. So strong recommend on listening to what your mother told you when you were growing up and resting if you feel ill.
Robert Wiblin: I think another thing that you can do that is good for society and good for you is to stop smoking. I don’t know what the exact data is on whether smokers have higher fatality rates here. I haven’t seen the latest on that but common sense would suggest that if it’s like other respiratory illnesses, that smoking is going to be an aggravating factor. More generally, I’m trying to get as much sleep as I can and just stay very healthy so that if I do get sick, I’m starting from a better base of health.
Robert Wiblin: And just in general, keep in mind that this is a war scenario for society. It’s a very serious issue and recklessness, going out, socializing in large groups: these are actions that seriously could kill other people and undermining what is a collective social effort to try to control this disease and get back to normal as soon as possible. Do you have anything to add on that, Howie?
Howie Lempel: I guess maybe one other thing I would add as far as those types of things that people can do or another reason why you really want to avoid transmitting a cold is you might be pretty sure that you don’t have COVID. Maybe you’ve matched up the symptoms and decided that it’s very unlikely. If you then you use that and then start going out, one big risk is that you get someone else a cold and then that cold, that person is going to spend the next two weeks wondering if they have this much more serious disease. They’re potentially going to spend those two weeks isolating themselves so that they know for sure they won’t spread it to anyone. And so just even if nobody gets sent to the hospital, the costs of getting someone else any kind of disease have just gone way up.
Robert Wiblin: Yeah. I might just add a little bit onto that about people who shouldn’t follow those instructions. I mean many listeners will be working in hospitals or they will be helping deliver electricity or collecting the trash or making the water function or delivering medicine to people in hospitals or just delivering groceries and essential items to people. Obviously those people, it’s impossible for them to stay at home. They’re the heroes who are keeping society functioning through this time. And hopefully they are getting instructions from their employer on how to minimize the risk to them and others of them transmitting the disease. I suppose obviously just trying to stay away from people and in some high risk professions, potentially wearing masks. But I guess we’ll leave that to people’s employers to offer advice on.
Robert Wiblin: Let’s just talk quickly about how you can try to get some idea of whether you have COVID or some other condition. I suppose in your case, Howie, you’re deciding to basically play it safe and regardless, to isolate yourself as much as possible. But we do have some ideas. Like if you think you have a 50% chance of having COVID on base rates, then you can look at your symptoms and potentially shift that estimate up a little bit up and down. Do you want to explain that?
Howie Lempel: Yeah, sure. So two of the symptoms that seem to be most common are dry cough and fever. And so that might be about when you start taking the possibility seriously that that’s what you’ve got. And there are some other symptoms that seem to be fairly uncommon in COVID relative to other similar diseases. Only 5% of people admitted to a hospital with COVID had a sore throat. Only 4% had a runny nose. 2% had diarrhea. So if all you’ve got is a sore throat and a runny nose, that’s a pretty good sign that you probably have something else.
Howie Lempel: If you’ve got a fever and a cough and a runny nose, you should certainly be taking the possibility that’s COVID quite seriously. But those are also pretty common symptoms. The runny nose makes it a bit more likely that maybe it’s something like flu where runny noses might be more common. And so that’s sort of the way that I would be thinking about figuring out how likely you are to be sick. But that said, I think being just on the cautious side, because it’s bad to spread any type of illness right now seems really important. And then the findings that we have on symptoms come from a study of a hundred hospitalized patients, so it wouldn’t be shocking to me if we had fairly different beliefs sometime down the road.
Robert Wiblin: Interestingly, I started getting cold symptoms a bit over three weeks ago. At the time, I estimated that there was kind of, given the number of people who start getting a cold or flu symptoms just every day regardless of COVID and given the number of people who we thought were infected in the UK, I think there was a base rate of about one in 3000 that had COVID. And then also, my symptoms weren’t ever a good match. So I had a runny nose and no fever. So that made it seem less likely. Then just a week ago I started getting cold symptoms again. By that stage, it seemed like the base rate had probably climbed potentially as high as one in a hundred. Fortunately, again, my symptoms didn’t match at all, so I don’t think that I actually have been infected.
Robert Wiblin: Fortunately, I’m also isolated out here and isolating myself. So fingers crossed, not passing it to anyone regardless of whether it is or isn’t. But it is interesting just how quickly this disease has spread such that a few weeks ago, the odds of you having it, if you had these symptoms was very low. But it is ramping up incredibly quickly.
What governments should do (Rob’s guess) [00:41:03]
Robert Wiblin: All right, let’s maybe talk about the situation in different countries. I actually spend a lot of my days at the moment looking over the case confirmation numbers, the testing numbers, the death numbers for different countries to understand which ones have the worst situation and which ones… well, the thing that I’m most interested in is finding out which countries are managing to successfully contain and suppress the infection and potentially turn things around.
Robert Wiblin: So as I mentioned, I guess things are very bad in Italy and Spain where they now have almost a full lockdown and people are not allowed to leave their houses unless they have a central business. Those countries seem to now have less than exponential growth, which is perhaps what you would expect if you were seeing a decrease in the number of contacts of people, starting a week or two ago, when people would have been exposed to the virus if they were now starting to get symptoms and get tested.
Robert Wiblin: Things are bad in France, Germany and Switzerland. They’re somewhat less bad in the UK, Australia and Canada. But they’re only days or a week behind. There’s other countries that are in a much worse situation. There’s only very limited breathing space for them to try to change things so that they don’t end up in the same situation that France, Italy, Spain, Switzerland are in now.
Robert Wiblin: It’s basically I think unknown what the situation is in the US because the testing has been so weak and as we mentioned, the testing in many poorer countries, many developing countries is basically completely absent so we just don’t have a clear picture at all. Is there anything you want to add on that, Howie?
Howie Lempel: No, that seems like a good summary to me.
Robert Wiblin: Yeah. Okay. And then the countries that are doing well. We have China, as we mentioned, which basically has suppressed the illness. South Korea, through massive testing, seems to have brought down the number of new cases below 100 each day and held it there. Singapore has a lot of testing and it also seems to have kept the number of new cases each day to about 10 or 20. There’s also Hong Kong, which actually I haven’t looked at that data in the last few days, so I’m not quite as familiar.
Robert Wiblin: A lot of people mentioned Japan. I was a bit disappointed to look yesterday and see that they actually had not been testing many people. So I suspect that the disease may be quite a bit more widespread in Japan than is appreciated and perhaps it’s a bit of a statistical illusion that they’re suppressing it as much as it seems. They had a 5% confirmation rate from memory, but they were like relative to the population of Japan; the number of tests was really quite low. Lower than in other places. So that’s a little bit concerning.
Robert Wiblin: Taiwan has done well despite the fact that they are incredibly linked with China. They had a very early response: manufacturing masks, discouraging people from going out, doing widespread testing, doing widespread contact tracing, preventing people from entering the country if they had, in the last 14 days, been in any region where COVID was prevalent. And so they have managed to bring down new cases to a fairly low and constant rate, and fingers crossed they’ll be able to keep it there.
Robert Wiblin: Someone was telling me that Kuwait has done a good job, but I haven’t had a chance to look at that yet. So that’s something that I’ll hopefully get to later in the day. Are there any other good news stories that you’d like to mention, Howie?
Howie Lempel: I think you’ve gotten most of the ones that I know of.
Robert Wiblin: Right. So I think what we can learn from this is that if you do the right combination of policies and you’re willing to pay the cost and to take action soon enough and you’re organized enough, this disease is controllable. I think there’s pretty good evidence of that now, at least for societies that can potentially do the kinds of things that China, South Korea, Singapore or Taiwan are doing, which I guess not every country can do, but I’m optimistic that places like the UK, Canada and Australia could do if they had the will and they started doing it as quickly as possible now.
Howie Lempel: That seems right as a proof of concept, but it’s still too early to see how. Both, I haven’t seen any great measures of costliness to compare it to and it’s still too early to see what happens as you roll it back. It’s definitely a huge win if all you had to do was tough it out for a couple of months. But that becomes a harder call as you go from there.
Robert Wiblin: Yeah. There’s a few ways that this could end up being mistaken I suppose. Yeah, as you mentioned, it could be that any loosening up of these restrictions means that you just get outbreaks again and so you’re kind of stuck in this constant bind where you have to keep imposing a high cost on people. Interestingly, in China and Singapore and Taiwan, they don’t have a lockdown. They don’t have lockdown conditions in South Korea. People are able to move around and life is continuing to a decent degree as normal. That is giving me some hope. I guess it’s possible that despite the fact that they’re doing quite a lot of testing, they’re still missing a lot of cases and it’s spreading under the radar and so it could be an illusion that that case numbers are as low as they are.
Robert Wiblin: What other ways could this… I suppose it could also just be the case that these countries are exceptionally more organized than other places and so other areas won’t be able to copy them. And then potentially, I suppose, somewhere like Singapore could just end up being overwhelmed by travelers from other countries bringing it in and that could exceed their capacity at containment and suppression and so they could end up failing in the long term. Is there any other ways that that lesson could end up being wrong?
Howie Lempel: Those seem like the main risks to me.
Robert Wiblin: It might just be worth me listing off again the things that I’m aware that these successful countries have done, especially the ones that were able to control cases without having a full lockdown. This is something that I’m researching a lot at the moment, trying to figure out, what is the pattern of what successful countries have been doing. So we might have more to say about this in a future episode or at least maybe in an article on our website.
Robert Wiblin: But basically South Korea, Singapore, Taiwan, they ramped up their testing capability very early and very aggressively. They developed places that people could go and get tested that were unlikely to then infect other people in the process of them getting there and waiting for the test results and so on. So they were able to test a lot of people from an early stage. They then had mandated home isolation for people who had tested positive or they kept them in hospitals. And they really did enforce that and would actually fine people and punish people if they violated those rules.
Robert Wiblin: In at least some of those countries, they also would chase up people who had had exposure to people who tested positive and then similarly, on pain of a serious fine or a criminal conviction, require them to remain in their rooms where they wouldn’t infect other people.
Robert Wiblin: Many of these places also increased… they stockpiled more masks than other places did and they have ramped up their production of face masks quite aggressively. I know there’s some skepticism among some people about the value of face masks, but there is an interesting pattern that countries that use face masks do seem to be doing better than countries that don’t. That could just be correlation or coincidence, but many of these countries do seem to think that people wearing face masks is an important aspect of their control strategy.
Robert Wiblin: Many of them imposed stronger restrictions on travel into their countries from regions where there were active cases of COVID demonstrated from an earlier date. For example, Taiwan started scanning people who were coming from Wuhan as early as the 31st of December for any cold symptoms, which is well ahead of what other countries, certainly what the UK or U.S. were doing. But that’s not surprising given how well connected they were with China.
Robert Wiblin: But they also cut off any connections from Wuhan and the rest of China quite a bit earlier than other countries did. They also actively were tracking down people’s travel history so they were able to find out whether people had been in those regions within the last two weeks and then deny them entry on that basis, whereas other countries have mostly lacked that capability.
Robert Wiblin: In many places they have also been able to use people’s phone records to see what phone numbers have had GPS tracking close to their phone, and then notify them immediately that they are required to stay home and self isolate. Which you can imagine there’s a risk that those people have been infected and then they immediately find out that someone they’ve met has had a positive case and then they go home and self isolate. That does make it a bunch harder for the virus to spread because you’re just, without having to keep everyone at home, you’re identifying most of the people who are most likely to have received the virus. Is there anything else you want to add on that, Howie?
Howie Lempel: Yeah. So one question is, do you have a sense of how many of those countries are countries that have had recent experience with just really serious respiratory illnesses, whether it’s sort of SARS or whether it’s MERS?
Robert Wiblin: Yes, all of them. Which may explain why they had all this infrastructure ready to go. And I guess that does suggest that it could be harder for other countries to copy. So Taiwan and Singapore both had SARS outbreaks and built institutions and processes in order to prevent a repeat of that including these kinds of tracking mechanisms. And I guess that could have been what prompted them to stockpile more materials for the situation.
Robert Wiblin: And South Korea had an outbreak of MERS, although I don’t know the details about that, which I think caused them to ramp up their testing capabilities. I’m trying to think are there any others? I guess Hong Kong was affected by SARS, similarly. China obviously was massively affected by SARS, which I guess in retrospect might have been a fortunate test run that has allowed them to do what they’re doing now.
Howie Lempel: And then I guess one other question that I’m very confused about when I think about comparisons across countries is why the U.S. and the UK seem to have been so unable to copy the parts of those strategies that seem most uncontroversial. Especially with rolling out testing. I mean as far as I’ve read, we basically have South Korea just way ahead of the United States having like seemingly unlimited drive-through testing while the U.S. is barely able to test anyone and still trying to manufacture its own tests. And I’m wondering if you have any insight into, I guess, both. What’s preventing the U.S. from moving more quickly and then also why is it not the case that as soon as this happens, the U.S. just buys IP from South Korea and just starts making the same tests?
Robert Wiblin: Yeah, I don’t understand the details of that. There does seem to be quite a big difference between the UK and Australia and the U.S. The U.S. seems to be doing exceptionally poorly in this regard. The number who were tested in the UK, I wish it were higher, but it’s at least a decent number. I think 20,000, 30,000 by now, which could be worse. Australia has actually tested 80,000 people when I last checked, which is actually quite a lot.
Robert Wiblin: The U.S., so I’m aware of part of the problem which was that the CDC said that they wanted to do all of the testing themselves and then they, I think, bought a bunch of tests and then they found out they didn’t work and then they tried to make their own and that didn’t work and they weren’t approving anyone else to conduct tests. And unfortunately, bizarrely during a pandemic, they have the ability to deny anyone else the ability to do tests for the disease.
Howie Lempel: My impression is that it was the FDA.
Robert Wiblin: Oh sorry, yeah. Sorry, I’m thinking of the government as a whole. But yeah, the FDA was blocking anyone else from rolling out their tests. And I think that has only recently kind of been relaxed, that they’ve started approving things. I mean, it’s one thing I understand… It’s to hard to run these projects, to scale these things up massively. It’s possible that any one institution might make mistakes and so they don’t manage to scale it up. But to forcibly, through your own regulatory power, prevent other hospitals, other research groups that can actually test people, that might save many lives and save trillions of dollars of lost GDP by controlling this thing. To use the law to prevent them from doing it just seems like an absolute barbarity to me. Made me furious and I think there’ll be a commission that will… hopefully heads will roll for this appalling decision.
Howie Lempel: My initial instinct is similar to yours, although I would really like to see any information at all about how accurate the other tests are. Maybe see where someone’s coming from. If you find out that the tests in South Korea actually don’t look so hot. But I suspect we’ll find out that they’re actually more than sufficient.
Robert Wiblin: Yeah, I mean it seems like they should be able to develop them and then roll them out and then in an emergency situation, then test later. Are they working once they’d actually started applying it, rather than having this very command and control centralized mechanism, which has this one single point of failure, the CDC, that then basically just can’t test people almost at all for weeks. Shocking.
Robert Wiblin: So much time wasted. Especially, it seems like different labs in different manufacturing centers around the world have had different approaches to producing these tests and it’s impossible for anyone to know ahead of time which one of these is going to have the best trade-off between cost and ability to manufacture them quickly and reliability.
Robert Wiblin: So they could really want lots of different groups to be trying to make these things. And then just whoever can make the most of them, start buying tons of it. But that was not the way the U.S. was thinking about it. Because I think a single university research lab in Washington, from memory, who managed to test more people than the entire federal government. There’s a single billionaire in China who sent more tests to the U.S. than the entire federal government has managed to provide up to now by a large fraction. So it gives you some sense of the scale of the failure. At least if their reporting on this is at all correct.
Howie Lempel: Yep, that’s right.
Robert Wiblin: Yeah. I expect that in terms of why other countries haven’t been able to do more, probably it is just a slightly difficult technical challenge to make these tests good and then manufacture very large numbers of them. I suppose if you have not done any of the preparatory work to figure out how you would do that. But I don’t know the details of… I don’t know the science behind it.
Robert Wiblin: I guess we talked about some ways that countries that we’re in, countries that many listeners are in, like the UK, U.S. and Australia, why they might not be able to copy. But I am somewhat optimistic that China, which has some very strong aspects of state capacity, but also some areas in which it’s weaker, did manage to successfully contain the disease, starting from what was really quite a high density of cases in Wuhan. Potentially like a large fraction of the population has already been infected. So it does seem worth it. Trying to give it a go to do that rather than just allow 1% of the population to die.
Robert Wiblin: And if we have a strong response now, then we can always decide later that it’s not practical and give up on that. Or we could learn from the experience of other countries that it doesn’t work in the long term. But if we don’t act very decisively and very quickly, then the door for that will close and we will just have to accept the very high level of fatality. And, of course, an enormous economic effect as well. If so many people are getting sick, if so many people are dying, I don’t think that is going to be great for consumer confidence. Of course, having to stay at home isn’t great either, but also just allowing very large numbers of fatalities will bring its own massive economic repercussions as well.
Robert Wiblin: I’ll just add that we’re talking about case studies in all these different countries: Italy, South Korea and so on. There’s a Wikipedia entry on the 2020 coronavirus pandemic in X for basically every country that is affected. Potentially just every country in the world by this point. Where you can often see a timeline of their response and you can see these nice graphs that show the increase in tests and confirmations and deaths and so on. So you can potentially learn about this yourself. There’s nothing magical that we’re doing here. Basically just requires the legwork of reading these things and trying to understand what’s happening in each country.
Howie Lempel: I guess in the story where you’re able to have a really short suppression period and then able to open up again afterwards and sort of from there, catch cases as they come up. That sounds like a pretty good story to me. I guess I worry about, one worry I have is just the other possibilities. At least some governments seem to be talking like we are going to have these intense measures and we’re trying to wait out a vaccine. And I guess I don’t feel like I’ve seen a lot of folks really look hard at how much of a talk to the economy are we really talking about here.
Howie Lempel: And who is this affecting? How are they going to make it through? And just really looking at that impact and asking, “Is it worth it to essentially shut down the economy for 12 to 18 months?” So I don’t know. Do you have any thoughts on, if the likelihood that that ends up being what the intervention looks like? And does it still look worthwhile if that’s what it looks like?
Robert Wiblin: Yeah, obviously I haven’t done all the modeling and the cost-benefit analysis there. I guess I’m not sure that anyone in the world has done that super well. I guess the Imperial College London study that we’ll link to might come closest, but that was obviously very rushed out the door, and there’s a lot more than one can say about it. It might be worth, at this point, me mapping out my view of what will happen over a longer period of time, so we can perhaps get an intuitive sense of how costly it will be if I’m right.
Robert Wiblin: So I think first, countries like the UK or US, where there’s already widespread community transmission, quite a lot of people have it. They’re going to have to enter a suppress phase, which could last, I guess, two to five weeks, which will be very costly. But the goal there is to bring the transition rate from one person to another well below one. So then over time, the number of new cases just starts coming down potentially quite a lot. More or less you have to do that, because otherwise if you don’t, within a few weeks, your country is already going to be overrun with cases. Then we can do the phase that China is in now, which I guess I’m going to call the release phase, which will happen potentially over one to six months, depending on how long it takes for us to learn how much we can get back to normal life.
Robert Wiblin: So obviously, during the suppress phase, we still have to keep supermarkets running. We still have to keep pharmacies running. We still have to keep the electricity grid running. But, during the release phase, we’ll figure out how much can we add back? How many people can go back to their offices? Can gyms reopen? Can people start going out on the street again? Without, the R nought figure, that is, the number of people who catch it from each affected person rising above one. If we can keep the R nought below one, then we’re in a stable situation, and we can just keep going with a relatively small manageable number of cases until we have a more serious solution to the problem.
Robert Wiblin: And it’s going to have to involve a bunch of learning on our part. How can we still have people having contact with one another without having lots of transmission? And fortunately, one advantage that we have is that we are going to be able to learn from the experience of other countries that are several months ahead of us. Countries like China, where they have been trying to figure out, how can they restart the economy, or how can they get things somewhat back to normal without lots of transmission. So things like just checking people’s temperature everywhere that you can so that as soon as people start showing a fever, they can self-isolate and potentially go to a special clinic where they can get tested quickly before they pass it on to other people.
Robert Wiblin: We’re already messaging a lot on hand washing. We’re going to have to keep that up a great deal just to have very high levels of personal hygiene and sanitation. These things like offices should be very well ventilated because that helps to clear out the air that might have these aerosolized virus particles in it. I guess, I don’t know how significant each of these individual things is, but probably together, they’re going to add up a fair bit.
Robert Wiblin: And also just massively stigmatizing people coughing in an uncovered way. It’s already a little bit rude in normal times. I think, at this point in history, it should be viewed as just a deadly thing to be doing in public. And so the hope is by adding those kinds of things, and then other things that we’ll learn from countries like Taiwan and China, we’ll be able to potentially have many, especially younger people, especially a bit healthier people who are less likely to get infected and also less likely to be killed by the virus, to go back to normal life. That’s one to six months period, I’m guessing.
Robert Wiblin: Then we enter this longer muddle through period, where I expect that having done as much as we can to get things back to normal, we’re going to sometimes have outbreaks in particular locations in cities, where it turns out that we’ve allowed R nought to slip above one and more people to start transmitting the virus and more people to catch it.
Robert Wiblin: And so we’re going to end up having to do this difficult balancing act between preventing outbreaks and having the economy function and not having a massive depression. But fortunately, over this time, we’ll likely have ramped up relevant medical training. We’ll have built lots of ventilators. We’ll potentially by this stage have quite effective treatments in terms of antivirals that, fingers crossed, we’ll be able to have manufactured a lot of. Hopefully the testing capability issues that we’ve had over the last month or two we’ll have resolved by then. And we’ll be able to have test far more people, and get the results much more quickly.
Robert Wiblin: And so that will potentially all make it easier to control outbreaks where they occur in particular locations. We might even have, in countries like the UK, figured out this mechanism for texting everyone who’s had exposure to someone who ends up getting diagnosed. That sounds like a technically complicated thing to do, but six months maybe if we really focus on it, we can do it.
Robert Wiblin: And through all of this time, we’re going to have researchers working incredibly hard, many labs converting over to working on a coronavirus vaccine, to working on testing antivirals to figure out which existing antivirals are most effective. And that, fingers crossed, will last only six to 18 months before we either get a vaccine, or very effective antivirals that do effectively mean the disease is rarely deadly, or potentially we now have so many ventilators and we’ve scaled up other treatments so well that we can relax and allow many people to become infected without freaking out too much.
Robert Wiblin: So that gives you some idea of the scale of the effort that we’re talking about here. And I don’t know whether that is more of an economic cost than most people expect it or less. We’re in for a pretty rough economic ride regardless, as I was saying earlier, and my hope is that this is the least damage approach.
Howie Lempel: How likely do you think it is that during the release phase we’re going to see something that makes us decide that this plan just isn’t that viable?
Robert Wiblin: Well, we might have a decent idea before we even get there because we’ll find out whether South Korea has been able to maintain control for more than a month. I guess maybe one in three. I guess I’m somewhat optimistic that if we keep a third of people who most don’t need to go back to work at home, and other people are doing everything they can, hopefully, out of fear of their own lives, quite literally, to avoid catching this virus, that we will be able to keep R nought at a sufficiently low level. Perhaps I’m just naively optimistic, but I guess I don’t feel like I’ve been naively optimistic about most other things so far.
Howie Lempel: That seems absolutely true.
Robert Wiblin: Do you have a more pessimistic take?
Howie Lempel: I guess I think that there is a world in which countries like the US, and the UK, and Australia are able to maintain very low levels of virus for a long time. I think I’m probably a bit more worried than you that it requires staying in a situation that’s similar to the suppress phase for a fairly long time, but I’m pretty unclear on whether or not we’re going to be able to start opening things up, and not have it just shoot up to another outbreak again. And countries have shown the ability to do it. I mean, if you lower the cases enough, then you’re able to just track every contact of anyone who does have it, and you are able to really cut down outbreaks that way. But whether or not these countries in particular can do it successfully, I think I’m a bit more worried.
Robert Wiblin: Okay. Interesting. So I guess a few responses to that. One is that even if we do end up abandoning this long term strategy, doing the suppress thing now and then trying to flatten the curve does still save quite a lot of lives, because in the meantime, we can potentially have manufactured some more antivirals, and some more ventilators, and have more ability to treat people without other people catching it.
Robert Wiblin: So every day of delay is very costly. But even if we don’t achieve a total victory, it can still be quite useful. I guess also we do always have the option of giving up this plan. So I guess the Imperial College London study tried to do a comparison of a more mixed strategy, which was just ask people to stay at home. Sometimes just do some control mechanisms. Try to reduce the rate of transmission so not everyone gets it at once. Comparing that approach with what I’m describing here, and concluded that there was a net benefit to doing what I was describing given their current estimates of how bad things are in countries that didn’t do that like Italy, versus how unlikely is it to work.
Robert Wiblin: But it could be that we decide that actually the flatten the curve approach, that middle ground, is the least harmful option. But it’s a one-way street. If we go for that, I think we’re not going to be able to turn back the clock and take the approach that I’m describing, but the reverse isn’t true. We maintain the optionality as long as we go hard now.
Howie Lempel: I think that that’s a great argument that overall I’m convinced by: for the approach that at least starts with suppression is we should at least see if people have the appetite to really bring this down to near zero, and then we should at least see what happens when we start releasing some restrictions. And you always have the option value to move back from that. But it seems just premature to see several different countries being so successful, and then to decide there’s no way we can possibly do that.
Robert Wiblin: Yeah, exactly. So just to give a sense of what would happen if we did nothing: the ICO study suggested that to reach natural herd immunity would need 50 to 70%, or something of the population to end up catching the illness. And if we did nothing to control it’s spread right now, they were saying a critical care bed demand would be over 30 times greater than the maximum supply in the US or the UK, which means that, as you were saying, effectively nobody who needs medical treatment will be able to get it. And then they estimated that about half a million people would die in the UK, which is about 0.75% of the population and about the same in the US. But of course, it could be quite a bit less or more than that. I wish I knew actually whether that was a mean, or expected value, or a median value, because it could be that the mean is quite a bit higher than the median in this case, but I couldn’t see that quickly.
Howie Lempel: Yeah, I’m not sure either.
Robert Wiblin: So I guess if I wanted to make the argument against this approach, maybe I would say even if you manage to delay it for a long time, you’ll have this inevitability of it bouncing back potentially in an even worse way in the next flu season, and suggest that it’s unlikely that we’ll have good treatments by then. I guess maybe that’s just another spin on the thing that you were saying, that it’s just too costly to maintain the level of suppression necessary for such a long period of time.
Howie Lempel: Is the reason that you get a bounce back in another flu season? Are you saying, a year from now, we still won’t have a vaccine, or are you saying, it’ll turn out that you just can’t build a vaccine against this? What does that look like where you get the bounce back?
Robert Wiblin: So I think a situation that looks quite bad in the modeling, and that has troubled some people is, what if we pay all these costs for doing suppression now. And then come next flu season, we haven’t really made progress on antivirals or a vaccine. We haven’t gotten there yet. But during flu season, we have a maximum rate of transmissibility of this thing. Plus we have normal flu and all of the other respiratory illnesses going around at the same time, increasing the fatality rate. And then at that point, we just find that we can’t control it sufficiently. It could be then we’ve paid an enormous cost now to basically just delay something that we could have allowed to happen now anyway. I think that is trumped by these other considerations, but I suppose that’s the way that things end up going particularly badly.
Howie Lempel: Yeah, that makes sense.
Robert Wiblin: One thing we might add is that it seems that there’s quite a bit of optimism about us finding antivirals that would reduce the symptoms of the illness. That there’s many, many trials going on with coronavirus patients all around the world. Trying to repurpose existing drugs that interfere with viral replication that people think might affect COVID. And they’re already showing some fairly promising signs. And I think it’s not unusual for antivirals to have usefulness across different kinds of viruses. Arguably, we already have found some tolerably good treatments, but I suppose we won’t know until we see replications and things like that, and longer term outcomes.
Robert Wiblin: Actually, one argument we haven’t made is that we don’t currently know how many people who survive the disease end up having long-term problems with their health. Things like chronic fatigue syndrome, or problems with damage to their lungs that potentially lower their quality of life for years or decades. And that’s something else that we will have a clearer picture of in a couple of months time, and where we might be glad that we did the suppression thing, and so, if we see that, in fact, the disease is worse than we thought, we can continue to pay a high price to control it. Whereas obviously, even if we find that out later, if we haven’t controlled it now, then that that option will have disappeared.
Howie Lempel: That’s a good point.
Robert Wiblin: I might just talk very quickly about some economic things given that I’m an economist. Suppose we don’t want to focus on this too much. But there’s actually surprising agreement among economists, I think, on what the government needs to be doing right now. At least the economists that I’m reading are in favor of doing a lot to stop the virus. Economists tend to be the kind of people who would bite the bullet and say, “Well, plenty of people need to die because just the cost will be too great to prevent it.” But I haven’t seen much of that from economists that I’m reading anyway.
Robert Wiblin: There’s widespread agreement that we need central banks to slash interest rates, which they’ve already done. Potentially rent and mortgage holidays as we mentioned earlier. And sick pay, actually: so many countries don’t have mandatory sick pay. So you have this terrible scenario where, say someone working in hospitality, someone preparing food, has to go to work even though they’re sick, which is a nightmare. And in countries that don’t already have mandatory sick pay or some system to allow sick people to pay their bills while remaining at home, we need to basically be immediately sending those people cash.
Robert Wiblin: Potentially tax holidays for employers, because many businesses are going to face severe cashflow issues here. And the government can potentially borrow and just lend them money effectively by not requiring them to pay tax, and thereby keeping them afloat and not destroy the structure of organized production that has been created here that will be very costly to put back together at the other end if we don’t preserve it now.
Robert Wiblin: Many economists, including economists who tend to be more conservative and not be in favor of the government just sending people money, currently think that the government should be sending people money right now, just immediate cash infusions in people’s bank accounts so that they can stay home. Expectations in the market of how much inflation we’re going to have, have fallen dramatically everywhere because people think that consumers like you and me are just not going to be spending very much money anytime soon because we’re so freaked out. And so potentially to get inflation back to where people expected it to be, so that we don’t place a crushing burden on people who’ve borrowed money with previous expectations of their revenue and what prices would be. Potentially those cash injections into people’s bank accounts should be wholly or partly newly printed money to try to just get more money in the system so you have more nominal spending.
Robert Wiblin: Is there anything else to say? Oh, I guess a more extreme measure that many countries are taking, including the UK, that I think many people would support is just emergency loans to insolvent businesses, or otherwise insolvent businesses. So airlines are going to take an enormous hit right now, but presumably we do want airlines to exist at the other end of this, and it seems like many of them are just not going to be able to continue, unless they get some kind of emergency financial assistance. I’m not sure exactly the extent to which you should take that, but it does make sense to me that given the governments in many places can borrow for next to nothing. Sometimes they’re even being paid to borrow, that they should do things to ensure that businesses that have very complicated internal structures that would take decades to put back into place don’t go under, because of contracts they signed before this huge shock. Do you have anything to add to that, Howie?
Howie Lempel: I agree with everything that you’ve said and I think you got most of it. I guess something that is, but I think it was less of an economic intervention, but might be some of one, is that there actually are huge supply needs at the moment, where we just desperately need to be manufacturing ventilators, to be manufacturing PPE. And so you can imagine if people are ending up being sent home from their factories, any of those can be retooled to do this type of work. Secondary factors like keeping people in their jobs.
Robert Wiblin: So there’s going to be potentially an enormous sudden restructuring that we need. So restaurants in many places are just going to be closed for quite some time. But fortunately, there’s going to be a lot of people who still want to eat food from restaurants. And so we’re going to need lots of delivery drivers all of a sudden, many more than we needed previously. People that are not going to want to go to the supermarket. So we need just tons of people figuring out some way to allow, say, one expert who knows how to not to infect themselves, who’s wearing a mask to go around and do shopping for many households.
Robert Wiblin: Amazon said that they’re going to hire 100,000 new people to deal with the increasing demand for, I guess, shopping not in actual shops. So, although many people are going to lose their jobs temporarily, and we need to adapt to that, there will be opportunities for some people to go and take what are incredibly important roles that help to stop the pandemic by allowing people to not leave their houses as much as possible. So potentially listeners could be among those people.
What you can do to help [01:16:33]
Howie Lempel: Okay. So now that we’ve given a bit of an outline of where things currently stand, we want to talk through a bunch of things that listeners and general people can actually do to contribute. Rob, you want to talk through the first couple of things?
Robert Wiblin: Yeah. This is something that I wish we had spent more time on already. We have some ideas, but many of these are somewhat speculative. So people should use their own minds and take with a pinch of salt, and also stay up to date on ways that this could be mistaken. I suspect that we’ll have future episodes where we discuss some of these options perhaps in more detail.
Robert Wiblin: I guess the first obvious one is to just share information to get everyone to take the threat as seriously as we’ll come across in this episode, we think that people should be. Most of my friends, most people who read my work I think are aware that this is an extremely serious situation, and we’re at war, and being asked to stay at home if you are not an essential worker is a reasonable price to pay to prevent what would be just a catastrophe.
Robert Wiblin: But many people who don’t read the news, don’t read Twitter, don’t listen to this podcast, this is perhaps coming as a bit of a shock to them, and they may not be as familiar with how pandemics function and exponential growth, and they may only have learned about this for the first time a few days ago. And for them, it’s very hard. I think, to adjust their expectations very quickly to go from thinking that they are about to go on holiday, say, they’re about to go on their trip to Italy to realizing that maybe they can’t leave the house for several weeks, it’s quite surprising.
Robert Wiblin: And it’s not surprising to me so much because I’ve been following this since late January. So it’s not surprising for us, because we’ve been paying a lot of attention. But if you have family and friends who are in that situation, who have not yet realized the dire situation that we’re in, in many places, having one-on-one conversations with them to explain all of the above, and passing them this episode potentially could save their lives, and could do a lot of good. And that’s something that can scale up to almost everyone can contribute to this effort.
Robert Wiblin: Something that you can potentially add into that is, there’s a bunch of pledges going around online where people sign up to do particular things like always wash their hands, cover their face in public, self-isolate inasmuch as it’s practical given their health and professional concerns. One that I’ve signed up to is the “STAND AGAINST CORONA” pledge; I believe it’s standagainstcorona.org. And you potentially sign that pledge and then share that with people on social media. I’ve been very active on social media trying to convince people to take this seriously.
Howie Lempel: Do you know what you’ve pledged to do?
Robert Wiblin: Yeah, I actually do. I can bring that up. So, it’s standagainstcorona.org, and I’ve pledged to clean my hands. So I wash my hands with soap often for at least 20 seconds. And if soap is unavailable, I’ll use hand sanitizer that contains at least 60% alcohol. To cover my mouth. So I’ll use my elbow or a tissue to cover coughs and sneezes, then throw out the tissue and wash my hands. I’ll keep my distance. So I’ll stay home when I reasonably can. And when I do go out, I’ll try to limit contact with others. And finally to care for others. So I’ll call and emotionally support people I know who are isolated or vulnerable. When I share information about COVID-19, I’ll do it without contributing to panic or stigma. Those are the four things.
Robert Wiblin: I mean one could go further, it’s not the most extreme pledge that one could make about this, but it seems pretty reasonable to me, somewhat easy for me, because I plan to be out in the country far away from other humans. So it’s not so onerous. But I think that’s something that will be sensible for most people to agree to do.
Howie Lempel: That sounds right to me.
Robert Wiblin: Another idea that I just had earlier today. So, we’ve been trying to think of ways that people can contribute, and there’s sometimes very impactful ways that people with very specific skills can contribute to. Obviously, for example, if you’re a vaccine researcher, maybe you should work on a vaccine for this condition. You probably know who you are, and have thought of that already. If you’re an expert on running trials for antivirals, those two things probably seem like the highest leverage pieces of work that are available in the entire world, but of course they’re not something that just randoms can jump into. There’s something that you almost certainly need specialized equipment and training in order to be able to do it all.
Robert Wiblin: But something that many people can do, I think is contact celebrities around the world and get them to post on social media to create little videos explaining why it’s very important to stay home. In terms of explaining these issues with exponential growth, and what a huge difference physical distancing can make. One way that I was thinking of organizing this is many celebrities now are getting diagnosed with COVID, and if each one of those then made a video explaining how important it is to control the illness, or if they were asked by their followers, or emailed asking them to produce videos, then that could help to create a constant stream of reinforcement for people.
Robert Wiblin: And I guess, in particular, some celebrities will reach people that this show doesn’t reach. If you have movie stars, singers, people who are on television regularly, talking about this, that could potentially cut through to a broader fraction of the population than you can get through Twitter or newspapers and so on. Do you have any thoughts on that?
Howie Lempel: Arnold Schwarzenegger has a public service announcement going around telling people to stay home that features his pet pony and his pet donkey. So Arnold at least is on our side. And it’s silly, but I think that that stuff really helps. That stuff gets shared. That stuff is popular across audiences. And so I think it’d be great to have more of that stuff.
Robert Wiblin: Yeah. Mel Brooks did a viral video today, and they’re reaching enormous audiences, potentially more people than a dire press conference which Boris Johnson does every day. So, if you’re in a position to just find the emails for these celebrities, or their publicists and so on, or just message them wherever you can get access, including, I guess, mid-tier celebrities, honestly, given that we would love to just have as many people do this as possible. And that’s something that many listeners would be able to do if they can’t find something else.
Robert Wiblin: Moving on, I guess, so we’ve talked about vaccines and antivirals, that that’s probably the obvious thing to do if you’re someone who knows how to. But something else that a wider range of people can do, I think, is write up reports on what methods seem to be working in other countries. It’s a bit surprising to me, but I have not seen very much analysis of this. I have not seen many people calling up people in Taiwan, even just ordinary people, or people with some exposure to the health system there to try to write up reports in detail of what they’ve done and what they believe works. And there’s, I guess a lot of issues that there’s sometimes just not very many contacts between the country that you’re in, and the countries where things are going well.
Robert Wiblin: And there’s a bunch of legwork understanding exactly what they did when, and digging into the data to find out whether it’s being controlled as well as it appears. There’s some subtlety here, but I think this is something that if you’re a research analyst who might be doing research in a bank, or in a government, then this is something that you probably can do from home. And then publicizing that work or merging it with the work of others to produce a clearer picture seems like it could be quite helpful.
Howie Lempel: And on a lot of these cases I’ve had trouble Googling decent reports on what exactly made South Korea so successful. And I don’t know if it’s the case, or there just aren’t reports, or if none of them are in English. So if you speak another language, going through and seeing if you can find sources that are good reliable descriptions of what policies were put in place, and which ones worked, which ones didn’t in various countries seems particularly valuable.
Robert Wiblin: There’s a real challenge here that governments are trying to put in place so many things very quickly. They’re absolutely run off their feet. The people who would maybe ordinarily be sitting down and doing this kind of research to figure out what should happen over a period of months, don’t have the time to do it. So there is a role for other people to collect this information and distill it in conversations outside of these institutions. And then I guess pass it on to people, or just have it become conventional wisdom in such a way that then informs policymakers who otherwise just don’t have the time to do the analysis themselves. It’s a pretty unusual situation.
Robert Wiblin: But it’s work that a think tank might be able to do, for example, and would be doing in ordinary times. And that becomes even more essential when so many people are trying to do implementation of policy and don’t have very much time to think about what the policy should actually be.
Robert Wiblin: So, if you’re someone who speaks South Korean, or you have friends who speaks South Korean, who can translate lots of materials, and then you can try to summarize them, I think that that could be very helpful. And this work needs to be done in each country somewhat separately. So the fact that, say, there’s materials in the UK perhaps that will end up describing what is working well in South Korea. That doesn’t mean that the French government is going to be picking it up. Someone else probably in Paris is going to have to do that legwork themselves as well. Does that sound right, Howie? There’s a sense in which it seems a little bit crazy for this to be the case, but I do think that that is the situation.
Howie Lempel: That’s at least my impression. I think there might be some challenges with like, you write up your thing, how does it funnel up to actually being seen by folks? But I think if people do a good enough job, there is really a reasonable chance of helping out with this type of thing.
Robert Wiblin: Well, one thing you can do, having written a report like that… So you want to publish it online and keep it up to date, and then you can integrate it into the Wikipedia article about the country’s response trying to add a section that interprets how good a job they’ve done of containing a virus in various different weeks and what they were doing at those times. The current Wikipedia articles on the pandemic outbreaks in each country are fairly good, but they lack that kind of deeper analysis, which I think would be helpful. And I’m sure that many people in government are reading the same kind of materials that we are to try to make sense of this.
Robert Wiblin: So making sure that they’re accurate and sophisticated, that would be very helpful. And just making sure that there’s a link in the Wikipedia article to the best analysis out there on that interpretation. Just another thing to add is, if you’re a retired doctor perhaps, or you’re someone who has medical experience, but isn’t currently practicing medicine, there may well be roles for you in scaling up the provision of treatment if the pandemic does run out of control.
Robert Wiblin: There’s complications here because maybe you don’t have the relevant training and you could end up doing things incorrectly, or being potentially a burden on colleagues if they need someone to run ventilators and you don’t know how to do that. So apply your common sense and some care. But I know that many healthcare systems are asking people to come out of retirement and they are asking dentists to come across who have substantial medical training and do things outside of dentistry in order to help with this crisis. So I guess, yeah. Use your brain and figure out whether there could be a role for you there.
Howie Lempel: Yep. That sounds right. And then I guess one particular constraint that we’re going to run up against, as we’ve said a few times, is having enough ventilator capacity for everybody who needs some. And so one version of that is having enough of the machines and it seems just incredibly urgent that the manufacturers who are already making these, that the government just use anything possible to pay them to scale up, and if there are factories that could be converted into making these, that also sounds great. It’s a little hard to just become a manufacturer doing ventilators on the spur of the moment. But people have started putting some effort into making scrappy alternative ventilators, finding alternative options like supplying O2, using O2 concentrators, which might not be as good, but might be better than nothing. If you do any of this, you have to be incredibly cautious because it is really easy to hurt someone by doing any of this wrong.
Howie Lempel: But to the extent that you are an engineer and know what you’re doing and have some experts involved you can work with, then getting the machinery in the hands of people who know how to use it seems like maybe a win. And then the other big constraint is going to be the people who know how to use it. And they’re not easy devices to use. And I’ve seen some models saying that the actual bottleneck is not going to be on the machines. It’s going to be on staff who know how to use them. So right now, honestly, I don’t have the experience to know how one might get trained to be able to use a ventilator and think you really want to avoid sort of flooding in to busy people instead of making tons of asks to find ways to help out. But if there’s somebody out there who would have the capacity to train tons of people to use ventilators, I don’t know what all the details and sticking points would be, but it would be great if somebody was thinking that through and seeing if there’s a way to do that.
Robert Wiblin: Yeah. I think we both heard operating a ventilator to protect someone who’s at risk of death is quite complicated. This is not by any means simple. This requires not only someone to have nursing training. They have to have ICU nursing training to do this specifically. So if you’re the kind of person who is close enough that you might be able to learn how to do this within a reasonable timeframe, you probably already know that. So this would be someone who’s a practicing nurse, perhaps, who never particularly learned to use a ventilator or hasn’t worked in an ICU yet, but feels like they could pick it up quite quickly, or someone who has done this in the past but needs to take a refresher.
Robert Wiblin: Yeah, my impression is that there are quite a lot of groups working on trying to figure out, firstly to scale up production of existing ventilator designs, but also find other ways of repurposing normal materials to make makeshift ventilators. It almost looks like, I guess you were saying these models suggest that that side is going to be sufficiently successful. That the tricky part is going to be training enough people to operate them, which seems pretty plausible. Another downside that you didn’t mention is that if we bring back retired workers, they’re especially vulnerable to catching the illness and potentially dying of it. So this is something that I think we’ll look into more to understand better who might be able to do this, who can we kind of recommend to take a greater interest in this and is it actually a good idea, on balance.
Robert Wiblin: And just on the oxygen supply thing. Apparently the issue there is that oxygen supply isn’t as good as full ventilation, but one medical professional can help several people access just concentrated oxygen in a way that one person can’t run multiple ventilators. So inasmuch as the bottleneck ends up being access to staff, then that’s one way that you can supply something that might just be good enough for many people without having to occupy so many medical professionals. Speaking of the issue of people, you know, medical staff catching COVID, another approach that people could take, which requires some expertise but potentially not full expertise, is to work on personal protective equipment. To try to find ways that we can scale up production of those or repurpose materials to have face masks that maybe aren’t optimal but reduce transmission rates somewhat or find ways to make more gloves. All of these kinds of things.
Robert Wiblin: Do you have anything to add on that, Howie? I saw one group that was working on this today, but I haven’t yet looked into them, so we’ll stick up a link to that, at least if it looks any good. This is another thing we mentioned last time that could be quite useful, is finding ways of taking personal protective equipment that’s been used and cleaning it or deactivating any viruses on the surface such that it could be used again safely. Of course, a lot of risks there if you do that inappropriately. One option, for example, would be heating. Another might be UV, but then you need to make sure that you aren’t destroying the property of the materials themselves that is protecting you. But that’s something that someone with relevant engineering or manufacturing experience might be able to to get into.
Howie Lempel: Yep, that sounds right. Another thing which we’ve talked about a little bit is just helping to teach people how to avoid contracting the illness and how to avoid passing it on and I don’t know, depending on exactly what your social network looks like. I think mine personally is just overloaded and saturated with messages about washing your hands, but that doesn’t mean that everyone else’s is. And so figuring out which of your relatives, which of your friends, might not know best practices and have that conversation with them about hygiene seems really valuable. If you find ways to scale that, that seems more valuable still.
Robert Wiblin: Yeah, that seems right. I guess it would also be helpful to have people in our broader social network trying to interpret the evidence that’s out there on how are colds and flus, and potentially this virus as well, most often transmitted. I found it surprisingly hard to… It’s possible that we just don’t know, but what fraction is transmitted through surfaces, what fraction is transmitted through coughing, how reliable is hand sanitizer for cleaning people’s hands if they don’t have access to soap and water. There’s a bunch of basic facts here that it’d be great to have people, I guess, pouring through literature making sense of that if they have the relevant research ability.
Howie Lempel: Yeah. I’ve often come into situations where I understand that there’s no research on COVID-19 in particular, and then so I’m hoping that there will be research on what’s a reasonable prior to have for a respiratory virus in general. And often it’s like, I personally, with the lack of background I have, often can’t find that type of thing, but it would be sometimes really informative.
Robert Wiblin: Yeah. That suggests that the bar might be moderately high that someone might have to have scientific or medical training. But I guess lots of listeners do have that. I guess another thing that many people can potentially contribute to is helping people who they know who become sick or otherwise vulnerable to maintain physical distancing just in practical terms. So going and doing shopping for them or collecting their medical supplies or helping people out financially. That’s one that we didn’t mention that many people are going to have cashflow issues here. Friends and family of yours might struggle to make ends meet if they are becoming unemployed, or aren’t getting paid right now if they were on casual hours. Obviously, there are issues lending money at any point to friends and family, but it seems like this is a particularly potentially good act right now. If you can ensure that someone is able to remain at home rather than go out and infect other people by lending them money in the hope that they’ll be able to pay you back when things return to normal. That’s a very kind thing to do.
Robert Wiblin: Another quick one is… I’ve been trying to look into, is there a threat to food security in places like London or in places like San Francisco? Is there a risk that supermarkets won’t be able to supply food? The best evidence I’ve been able to get is no. That people in the area do believe that food security remains high. That there’s not going to be a shut off of trade of food between countries and that the supply chains and the logistics are still working quite well. And the only reason that they’re out of stock right now is just that people have, basically tons of stock has been transferred from supermarkets to people’s houses and pantries, but that things will return to normal in due course.
Robert Wiblin: Nonetheless, I personally am doing everything I can to avoid wasting food right now. I think inasmuch as we have already during this disaster situation managed to get food from the farm into people’s houses, we should not be squandering it because we are a bit unsure what the future holds and we ideally don’t want to. We want to have as few people having to do that work as possible, which we achieve if we don’t throw out food.
Howie Lempel: Is there anything else to add on how people can contribute?
Robert Wiblin: Hopefully, I think we’ll have more to say on this and certainly more to write about this on the website in coming weeks.
Howie Lempel: I’m all out at the minute.
Robert Wiblin: Sounds good. All right. Well get emailing your celebrity friends, everyone.
The bigger picture [01:37:19]
Robert Wiblin: I guess, actually one thing in the bigger picture that we can add is just this week, we published our global catastrophic biological risks problem profile, which is a new, fairly long and detailed article about how you could potentially contribute to preventing very bad pandemics from effecting humanity and taking it off track. The focus is on pandemics that are even worse than COVID-19. Pandemics that don’t just threaten to kill 1% of the population, but could kill 10 or 50% of the population. And those, while they’re somewhat unlikely, are just not that much less likely than what we’re seeing now with COVID-19. We’re in some ways fortunate that COVID-19 doesn’t have an even greater virulence and doesn’t kill a larger fraction of people. So I can definitely recommend reading that. And we’re going to have an interview with the author of that article, Greg Lewis, hopefully coming out pretty soon. Is there anything that we should say about how society could have better prepared itself for this situation, Howie? I suppose I’ve been complaining about this on my social media feeds.
Howie Lempel: Yeah, I guess it depends at what kind of time period you’re thinking of. I think that there’s been a problem for decades where being prepared for a pandemic, it’s just, I think one of the most valuable functions that a government can play. There’s just nobody else who’s going to be in a place to really be pouring resources in advance to try to get us prepared. And so everything from work to detect new outbreaks earlier on. Even detect them in animal populations before they’ve transmitted over to humans. To building better diagnostics. To coming up with faster processes to get from recognizing a novel pathogen to having a vaccine: right now, we think that’s 12 to 18 months. That’s just sort of unacceptable. We knew that that was unacceptable 10 years ago. There’s work being done on it by incredible people and governments certainly fund it.
Howie Lempel: But I think that at basically every point, there were tons of opportunities where it was clear more resources could make a difference and we never quite had enough. I think often there’s a problem where this type of thing will get attention right after an outbreak and there will be a bunch of changes that are geared especially towards something that’ll be useful for that outbreak in particular. So we get lots of better Ebola diagnostics after the Ebola outbreak, but it’s hard to sustain funding for things like platforms for in general manufacturing or researching and developing vaccines more quickly, because you can’t picture the way that will help. But as we’ve seen, when a novel virus comes out of nowhere, those are the times you’re most at risk. So it’s really important to have the sort of flexibility to be able to respond to those. So yeah, so on a sort of years to decades scale, I think that there’s a lot that we could have done to prepare earlier.
Robert Wiblin: Yeah, definitely. There’s a lot more to say about that, that we do say in episode 70 with Dr. Cassidy Nelson on the 12 best ways to stop the next pandemic (and limit COVID-19), and we have three other episodes from a couple of years ago, including one with you, Howie, where we talk about what society could have done to prepare. And this is going to be an incredibly hot area I think in years to come. We’re going to see a lot more money flowing into public health, a lot more money flowing into pandemic preparedness. So this could potentially be a problem that we should see many listeners flow into to fill those roles and to make as big a contribution as they can to make sure that we never face this situation again. So seriously, if you’re at a crossroad in your career or not sure what you want to do, this is something you should seriously be considering doing, I think, because there’s going to be many different angles. Economists, medical people, social scientists, people in government, policymakers, advocates. All of these roles potentially can help to control pandemics going forward.
Robert Wiblin: And we will have more content to talk, not only about COVID now, but the bigger picture for pandemic control in the future. Just giving a narrower focus for one second, I started getting worried about COVID-19 around the 20th of January and I think you were the same. Admittedly, we have some expertise in this area. We’re the kind of person who’s read several books about pandemics, so perhaps not typical. But I was already stockpiling food on the 27th of January and hand sanitizer as well. And I think you were in the same situation. I have been incredibly frustrated that public health professionals, that epidemiologists, that governments did not tell people to do this sooner. I understand that they are concerned about inducing panic, but we were able to see, you and I, we’re not super experts on this. We’re only moderate experts, and we had other jobs to do. We were doing this only part-time. We could see that there was a decent chance that exactly what has happened might happen.
Robert Wiblin: And presumably there are some people in government who knew this. Some experts who knew this. The alarm could have been sounded a lot sooner and we could have had five extra weeks to prepare. Five extra weeks to stockpile food. Five extra weeks to manufacture more hand sanitizer. Five extra weeks to make more ventilators. Five extra weeks to train people to use the ventilators. Five extra weeks to figure out what the policy should be if things got to where they are now. Work was done in that time, but I think a lot less than could have been done if we had had just the forecasting ability to think a month or two ahead, and to think about probabilities and expected value. And this is another area where I think we could improve a great deal.
Robert Wiblin: I suppose we probably won’t fall for this exact mistake again. Probably the next time this happens, the world will completely freak out everywhere simultaneously. But we need better ability to sound the alarm, potentially greater willingness actually on the part of experts to say, “I’m very concerned about this and people should start taking action, not panic, but measured action now to prepare,” because otherwise it’ll be a different disaster next time and we’ll have sat on our hands for weeks wasting time that could have saved lives. Do you have anything to add to that?
Howie Lempel: I think one thing that we need as a society, although I don’t know how to get there, is an ability to see an expert say that they are really concerned about some risk. They think it likely won’t materialize, but it is absolutely worth putting a whole bunch of resources into preparing, and seeing that happen and then seeing the risk not materialize and not just cracking down on and shaming that expert, because that’s just going to be what happens most of the time if you want to prepare for things that don’t occur that often. And right now, we just have a set of incentives where I think public health folks, epidemiologists, have to be really brave to call for big preparations because if they’re wrong, it’s sort of like egg on their face, and that’s not really the right way to think about forecasting.
Robert Wiblin: Yeah. People have to be able to say there’s a 20% chance that this will be terrible. That is sufficient reason to maybe have a few weeks worth of food in your house so that you can engage in physical distancing if it becomes necessary, but it doesn’t mean that it’s a certainty and that food may not end up being absolutely necessary and instead you can just eat it in the normal course of events because having several weeks of food in your house isn’t that bad. Or we should increase manufacturing of hand sanitizer. It’s just, there’s a real asymmetric risk issue here where I feel like preparing ahead of time for a lot of this stuff is just not very expensive, whereas it’s disastrous if you find yourself caught at the last minute without having done it.
Howie Lempel: Well, I think the argument for a bit more cost on the preparation side, is that I think the experience with pandemics or outbreaks that never got to this level, has been a bunch of experts say we need to really call attention to this. It’s being ignored. There ends up being a lot of public attention. People end up just associating it really strongly with whatever location the outbreak happened at and now maybe you have stigma against that location. Maybe their tourist industry drops because you don’t want to trade with them for maybe years over something that ended up being nothing. And I think we just need to find a way to stop that effect from happening and also to say sometimes the risk that’s coming is just big enough that you have to eat that cost and take that risk. I guess just have some empathy for where people who are being more cautious are coming from. They have seen, several times, like lower middle income countries, economies get really damaged by warnings about epidemic that never really materialized.
Robert Wiblin: Yeah, I guess I do weigh that up against the fact that this is now potentially going to kill millions of people, possibly tens of millions if we hadn’t had a proper response. Or if we weren’t starting to do that now. It’s going to cost tens of trillions of dollars potentially globally to stop this. I don’t want to see Wuhan stigmatized and there’s no need for that. But at the same time, having that happen a few times and then saving tens of trillions of dollars and millions of lives, maybe we do just have to eat that cost as you’re saying.
Howie Lempel: I guess the other worry there is just sort of the game theory, where if you do that too many times and countries end up paying that penalty too many times, then they have more and more of an incentive to hide outbreaks for a longer and longer period of time. And so I think that’s sort of like another risk there. But overall, I agree with you. You really want to get rid of this factor, but even if you can’t, you just can’t sit around while a pandemic is coming.
Robert Wiblin: Yeah. My guess is many people don’t realize the scale of the potential costs, whereas we were aware of that. I suppose, I think epidemiologists should have been aware of it, but perhaps it wasn’t in the front of the mind for them. But yeah, I guess the public is somewhat to blame that people do worry about calling out disasters that then don’t occur and having their reputation damaged. Listeners, next time you hear an expert say that something might go really wrong and then it doesn’t, you should not dismiss them. Not think less of them. Because it’s part of the role that experts play, is to have enough understanding, to sound the alarm before the probability is 100% when the probability is 10% and we need to start taking early action.
Robert Wiblin: All right. I guess to me this seems like it could be one of the most important things that ever happens during my lifetime. It could have a huge effect on international politics. It’s having a huge effect on people’s lives right now. I’ve tried to think back to what is the previous most important event in human history in terms of a global news story, and I thought potentially the fall of the Soviet Union and the end of the Cold War could end up being the previous most important event. Or, I suppose, we could all end up triumphing over this and perhaps this won’t look quite so big in retrospect. But I suppose that’s kind of my present guess. What do you think, Howie?
Howie Lempel: Geez, hard to say.
Robert Wiblin: Let’s engage in some totally errant speculation that no one has asked us to do.
Howie Lempel: It seems like it’s got a shot to be an event that’s really remembered. I think especially if it has big effects on political systems. So I think September 11th changed the way that the United States government worked for a pretty long time and changed its foreign policy focus. Changed what civil liberties Americans were and were not willing to give up. And a lot of elections really were about who’s toughest on terrorists. And so I can imagine something analogous where, are you going to prevent this from ever happening again? Are we going to be prepared next time? Ends up being a really important part of politics going forward for some limited amount of time.
Robert Wiblin: Yeah. I guess I’ll try to finish on a positive note. In fact, I won’t have to try that hard because I do have a lot of optimism here. I really do think that the UK, probably also the U.S., countries like Canada, Australia, do have the chance to basically win over this disease, to go through the suppression phase, to then muddle through what will be admittedly a difficult time where there’ll be some fatalities and there’ll be some economic damage, but then to get through to the other side where we do have sufficiently good treatments and we do basically win a measured victory over this. There’s lots of ways that people can contribute beginning with just staying at home and not falling victim to it themselves. I’m optimistic that there’ll be moderately good treatments that will be available within a year and just given the sheer number of people working on a vaccine, I think they have a decent shot at coming up with a vaccine within a year or two.
Robert Wiblin: So horrible though things look, I think there’s lots of reasons to be hopeful that humanity can really pull together here and use technology and science and good policymaking to save a lot of lives and to reduce a lot of economic damage. I’ve also been impressed with the speed of the economic response. I think a lot of governments are doing the things that we suggested and they’re doing them very quickly, so that’s really great. The area that I’m not sure about is poor countries that don’t have the state capacity and don’t have the technological capacity. I just haven’t been focusing on that just yet, but we will get to it. I’m hopeful that we will be able to find a positive take on that as well, but potentially not, in which case that could be a very sad story and something that we need to focus much more on responding to in coming weeks.
Howie Lempel: I don’t think I can follow up on that with anything worthy. I agree with Rob’s take that there’s a bunch of reasons for optimism and we’re just going to have to see how it goes over the next few weeks.
Robert Wiblin: All right, fantastic. Well, my guest today has been Howie Lempel. This has been an emergency episode of the 80,000 Hours podcast and we’ll be back with more COVID-19 material as soon as we can figure out our conclusions and produce it. Thanks so much.
Howie Lempel: Thanks Rob.
Related episodes
About the show
The 80,000 Hours Podcast features unusually in-depth conversations about the world's most pressing problems and how you can use your career to solve them. We invite guests pursuing a wide range of career paths — from academics and activists to entrepreneurs and policymakers — to analyse the case for and against working on different issues and which approaches are best for solving them.
Get in touch with feedback or guest suggestions by emailing [email protected].
What should I listen to first?
We've carefully selected 10 episodes we think it could make sense to listen to first, on a separate podcast feed:
Check out 'Effective Altruism: An Introduction'
Subscribe here, or anywhere you get podcasts:
If you're new, see the podcast homepage for ideas on where to start, or browse our full episode archive.