#4 – Howie Lempel on why we aren’t worried enough about the next pandemic — and specifically what we can do to stop it.
#4 – Howie Lempel on why we aren’t worried enough about the next pandemic — and specifically what we can do to stop it.
By Robert Wiblin and Howie Lempel · Published August 23rd, 2017
What natural disaster is most likely to kill more than 10 million human beings in the next 20 years?
Terrorism? Famine? An asteroid?
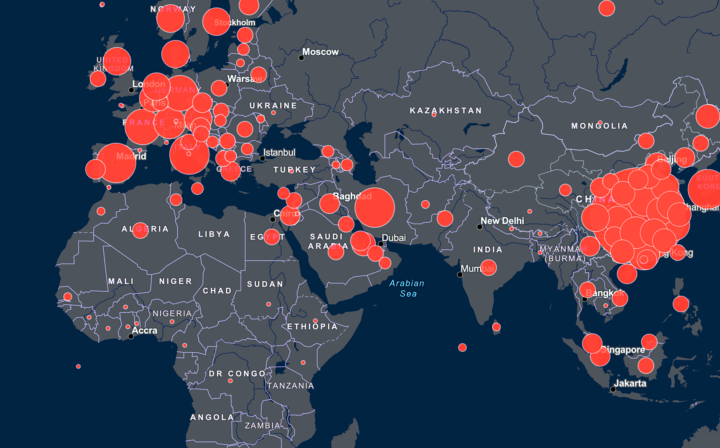
Actually it’s probably a pandemic: a deadly new disease that spreads out of control. We’ve recently seen the risks with Ebola and swine flu, but they pale in comparison to the Spanish flu which killed 3% of the world’s population in 1918 to 1920. If a pandemic of that scale happened again today, 200 million would die.
Looking back further, the Black Death killed 30 to 60% of Europe’s population, which would today be two to four billion globally.
The world is woefully unprepared to deal with new diseases. Many countries have weak or non-existent health services. Diseases can spread worldwide in days due to air travel. And international efforts to limit the spread of new diseases are slow, if they happen at all.
Even more worryingly, scientific advances are making it easier to create diseases much worse than anything nature could throw at us – whether by accident or deliberately.
In this in-depth interview I speak to Howie Lempel, who spent years studying pandemic preparedness for Open Philanthropy. We spend the first 20 minutes covering his work as a foundation grant-maker, then discuss how bad the pandemic problem is, why it’s probably getting worse, and what can be done about it. In the second half of the interview we go through what you personally could study and where you could work to tackle one of the worst threats facing humanity.
Highlights
Tens of millions could die in a pandemic during our lifetimes, perhaps even billions in a worst case scenario. This presents a serious risk to social stability.
Recent and historical pandemics show that we are not reliably good at controlling new diseases, and that they can often kill a large fraction of infected people.
Advances in biology makes it much easier to create highly dangerous diseases that could be even worse. Biosafety regulations reduce the risk of dangerous pathogens escaping the lab, but not to zero.
Local and international institutions for tackling new pandemics leave a lot to be desired. Fast response is essential to stop the spread – but it can take a long time to haggle over who is going to pitch in. Coordination between the many bodies meant to play a role is poor. Furthermore, it’s hard to transport qualified people and equipment to a disaster zone.
There are many opportunities to reduce the risk, in the government, private sector or charities. Many groups have proposed sensible ways we could better prepare ourselves for a pandemic but the suggestions are largely not being applied.
People can work to tackle pandemics with an unusually wide range of specialties – medicine, biomedical research, social science, security studies, and entrepreneurship. We suggest a number of places to study and work.
Articles, books, and other media discussed in the show
- What Bill Gates is afraid of
- These scientists are racing to prevent the next Ebola
- Jobs at Open Philanthropy
- Open Philanthropy grants for biosecurity and pandemic preparedness.
- Explanation of why Open Philanthropy works on biosecurity
- Ebola’s lessons by Laurie Garrett
- Ebola: Story of an Outbreak by Laurie Garrett
- A National Blueprint for Biodefense: Leadership and Major Reform Needed to Optimize Efforts by the Blue Ribbon Study Panel on Biodefense
- A Major Avian Influenza Outbreak Could Kill 62 Million People
- Our profile of the biosecurity problem
Transcript
Hi I’m Robert Wiblin, Director of Research at 80,000 Hours. Thanks so much for joining. The last few episodes have been really well received and it’s been gratifying to see our regular audience growing quickly.
If you haven’t subscribed yet, search for ‘the 80,000 Hours Podcast’ wherever you get podcasts. That way you’ll never miss an episode about something you’re interested in, can listen in while you’re cleaning or travelling, and can speed the conversation as you like.
Today’s episode is the longest so far – two and a half hours. But if you listen through you’ll know a hell of a lot about why pandemics are such a scary threat and what we can all do about them.
We’ve put an index in the show notes and the associated blog post so you can look through and skip to any section you’re particularly interested in.
So, enjoy!
Robert Wiblin: Today, I’m speaking with Howie Lempel, who, until recently was a program officer for Open Philanthropy, where he’s worked on problems including biosecurity and pandemic preparedness. For those who don’t know him, Open Philanthropy is a foundation whose goal is to make philanthropy go especially far in terms of improving lives. It’s the main philanthropic vehicle for Cari Tuna and her husband, Facebook co-founder, Dustin Moskovitz, who are expected to give about $8 billion over the course of their lives. And for disclosure, 80,000 Hours’ biggest donor is actually Open Philanthropy. But prior to working at Open Philanthropy, or OpenPhil, as we call it, Howie studied at Yale Law school and worked for the Brookings Institution and various criminal justice reform organizations. Thanks so much for coming on the show.
Howie Lempel: Thanks, Rob. I’m really excited to be here.
Robert Wiblin: So we plan to talk about the nature of the risks from pandemics, what can be done about them, and how listeners can best use their career to reduce the threat. But first, what did you work on at Open Philanthropy?
Howie Lempel: Sure. So when I started at Open Philanthropy, it was a brand new organization. It was like a mix between being a large foundation and having the feel of a smaller startup. That meant that at the beginning, everybody was a bit of a generalist. So when we started, our first major project was deciding what areas of philanthropy, what problems and causes seemed especially promising for OpenPhil’s giving. So from our first year or so, my main work was doing research to that end, and the questions that we asked to choose our program areas were: could we find causes that had a really big scope or scale of the problem that we were trying to solve, that really affected a lot of people and had a big effect in their lives, where it didn’t seem like there was enough philanthropy that already existed? And also where it seemed like there were concrete things that more money could do to help.
So we started with this huge list of all the causes that seemed like it could be potential candidates, and I was one of the people at the start who did really shallow looks at each of those causes. So, talking to maybe two or three experts and getting their sense of helping us understand what the problem was in that area, what people were already working on, what sort of important possible solutions there were that people weren’t working on yet, and start getting a sense of what philanthropy could do in the area. So my job at first involved both reading up, quickly getting to know a lot of different areas, and then going out and reaching out to the real experts in the field, and trying to get their sense of what more philanthropy would do in each of those areas. And over time, as we started to specialize, the job changed because we dug in more.
Robert Wiblin: So this is extremely similar to what 80,000 Hours does, or is part of what we do, and I think we actually copied the framework that you were using initially. So our problem framework is to look for issues in the world that are really large in scale, that not many people are working on, and where it seems like you could easily make a difference by spending more resources, so like scale, neglectedness and tractability we call it. We’ve relied on Open Philanthropy’s research quite a bit in forming our own list. So I guess the openness has been pretty useful for us.
Howie Lempel: Yes, I think the same types of questions that 80,000 Hours is asking, when they’re thinking about how someone can do as good as they can with their career, that’s the type of question that Open Philanthropy is asking, but thinking about how a foundation can do as much good as they can with donating money.
Robert Wiblin: And I suppose that there are some differences there between where you need talent to go and where you need money to go, but because they can convert between one another it’s a pretty similar problem.
Howie Lempel: Absolutely.
Robert Wiblin: A lot of what OpenPhil did in the early days is what we call our global priorities research, trying to figure out working on which problem you can have the largest impact with your money or your career, and I think in the future we’ll probably have a full episode devoted just to that topic. It’s one of our recommended areas because there’s very few people doing it and it seems like you can have a very large impact by shifting resources from problems that are somewhat less pressing for the world toward the problems that are much more pressing.
And potentially we’re not allocating resources in a very effective way overall because there’s just not many people who are trying to make these prioritization decisions, trying to figure out do you accomplish more good by focusing on health or education, or on these global catastrophic risks or something else completely different. So OpenPhil has been able to make quite a lot of progress in a short amount of time just by looking at something on which not a lot of people had already tried to work. Is OpenPhil a place that you would recommend people work?
Howie Lempel: Yes, absolutely. I think working at OpenPhil is one of the best career decisions I’ve made and I think it’s one of the best places in the world to work on cause-prioritization-type issues because I think it’s pretty unique in that it is open to so many causes and really cares about cause prioritization, but also has the resources to actually … Once it chooses a cause, make a real bet on that cause, and I think that that really is a good learning opportunity when you’re working on cause prioritization. So knowing that you’re eventually going to actually have to make a bet, and that the organization is going to make grants, I think it imposes some discipline on…
Robert Wiblin: Focuses the mind.
Howie Lempel: Yes, I think that that’s right, and then also I think there are certain questions that it forces you to ask about, “How much money could this field absolutely absorb?” Like, “Are there good reasons why X area is neglected? That you would only know if you talk to potential grantees.” That type of thing, that it’s pretty hard to get if you’re not in the position of grant-maker. So I think it’s a pretty unique place to do that type of work and, yes, I’d definitely recommend it for people who are interested.
Robert Wiblin: Do you know if they’re hiring at the moment?
Howie Lempel: I don’t.
Robert Wiblin: Okay, yes, well we’ll stick up a link to their vacancies page. I don’t know whether they’re hiring right now but they might well be at some point in the next six months, so yes, you can potentially get on their mailing list and find out about that. What was your research work at OpenPhil like day-to-day?
Howie Lempel: It depended on exactly what task I was working on, but a lot of the work was first spending as much time as I could really talking to experts in the field and learning from them. So it’s a lot of phone calls reaching out to top people, reading and trying to get to know a field well enough that I knew, and advise quickly as possible the main open questions that would affect whether or not we wanted to enter a cause area, and then try and figure out mostly through Internet research, academic research, who the people were who could answer those questions, and then trying to reach out to them and look at their answers.
Then once we identified areas as particularly promising, the work changed a little bit, and there were some cause areas where the next step was really to go out and find grant-making opportunities. That meant a lot of going to conferences, getting to know everybody in the field, trying to understand what role every organization played, whether there were things that seemed like gaps to us, types of organizations that really ought to exist and didn’t, or organizations whose work we would really like to expand, and then go out and make friends ourselves. Sometimes, for program areas where we really felt like we needed an expert or a specialist to scale up our grant-making who had … Instead of whatever amount of expertise I can get in a few months of learning about an area, there are people who have spent years and years building up their networks and expertise.
So sometimes my job is to find that person and go out and trying to recruit someone. And again, that actually involved relatively similar work. The difference between taking a bet on an individual who you’re going to then give the responsibility to do overt grant-making, versus taking a bet on the organization you’re going to grant to is pretty similar. So it’s a lot of going out into the field, making sure everybody knows my face, going to conferences, getting to know people, and getting them to … building up trusting relationships that you could ask them for their advice on who we ought to hire to go and run a program area.
Robert Wiblin: So did people suck up to you a lot because you had a lot of money to give away? Was it hard to know who to trust?
Howie Lempel: Yes. I think that’s one of the hardest parts of working for a foundation, is there’s a pretty awkward relationship where you have a lot of power, and people really do want to please you, and it takes a lot of work to build a trusting relationship where people feel like they can give you negative feedback, people feel like they can be honest with you, and yes, I think that’s a major challenge working at a foundation.
Robert Wiblin: So do you think the work had a large impact?
Howie Lempel: I really do think it did. I think that there are relatively few foundations like OpenPhil that are large and have that level of resources, and that also have OpenPhil’s openness to really going into almost any cause area where it feels like it could make the biggest difference. So I think that OpenPhil really was able to find some areas where there was nobody available to give the kind of philanthropy that was needed and really make a big difference. So one area that’s really important to me is working on reducing the suffering caused by factory farming. And OpenPhil was able to enter that area and become really one of the largest donors in that area.
And similarly, in the area that we’re talking about, pandemics and biosecurity, it’s an area where there’s a lot of funding by governments, but there are certain activities that really can’t be done by governments, so something like political advocacy or policy advocacy often can’t be done by governments. It’s sort of certain really sensitive questions that governments often can’t really work on, so I think it’s really important to have private sector money in there to hold governments accountable. I think that’s something that OpenPhil really was able to do in an important area and it was really clear that there weren’t many other foundations in the area available to give that kind of funding.
Robert Wiblin: You’re saying in a sense that the field isn’t neglected in terms of what governments can do, or not so neglected, but then in terms of what independent actors, nongovernment actors can do, that those things often aren’t getting done because there’s just no one there?
Howie Lempel: Well, I would say that there are two issues. One of them is exactly what you said. It’s an area where … Public health is one of the big priorities of a lot of governments, so there is a lot of spending in that area by governments. There is almost no spending on things like policy advocacy, think tanks. The whole NGO sector that usually exists in important policy fields was really neglected, then there’s a second issue, which is my … The main thing that I care about in this area, and OpenPhil’s priority, was in particular, reducing the chance of the worst-case scenarios among pandemics. Things that can really be what we called global catastrophes. I think that that’s something that governments often aren’t quite able to focus on as much as we might like.
They often work in very short time cycles. Congress has to renew funding every couple of years for most agencies so it’s really hard for governments to focus on the long run, focus on things that might not be likely, but that would be a really big impact if it were to occur. I think that if you want governments to be able to work on those types of things, you really need some advocacy to back them up, sort of subsidize that work from the private sectors. I think we’re both able to fill that gap in the private sector, that there wasn’t that much philanthropy, and then also I’m hoping that Open Philanthropy will be able to support the government through advocacy and allow it to really prioritize some of the stuff that we thought was most important.
Robert Wiblin: Does OpenPhil work on any other problem areas where the situation is similar?
Howie Lempel: I actually think that this was pretty unique among OpenPhil’s cause areas, at least while I was there. Because OpenPhil really does prioritize areas that are both very important and also neglected, often that meant it was areas that were neglected even by the public sector. So biosecurity and pandemic preparedness stood out to us as an area that was a little bit different, because it does have relatively large amounts of spending by governments but that still seemed like there were big gaps. The other thing that’s sort of unique about this area, is that it’s a little hard to define exactly what counts as spending through these pandemics.
So there’s a lot of work on public health in general that would be helpful from the perspective of pandemic preparedness, but that maybe isn’t the top thing that you might prioritize if all you cared about was using risk from pandemics, or in particular reducing risks from the types of pandemics that could really be global catastrophes. So if you look narrowly at interventions that are specifically focused just on lowering risk from that type of pandemic, then even governments I would say really neglect that.
Robert Wiblin: So there’s just general public health spending designed for disease control that is better than nothing, but it’s not the thing that you’ve been most interested in doing if you were just focused on preventing a pandemic that could kill a really large number of people and was completely new.
Howie Lempel: Exactly.
Robert Wiblin: What kind of grants did you make in the area while you were at OpenPhil? Or what grants did OpenPhil make?
Howie Lempel: So the main priority for most of the time I was there was actually not grant-making, but it was getting to know the area really well, start to set our strategy, and we made our hire, somebody who’s an expert in the field, Jaime Yassif, who’s now running the program area. But we did make a couple of grants while I was there. One of them was to a Blue Ribbon panel on biodefense in Washington DC. We gave them, to start, for their first year about $300,000 of our funding. They also had a bunch of other funding from other organizations. What they did was they got a panel of real policy luminaries, former policymakers in DC, to convene a set of meetings and identify real priorities in United States biodefense policy.
So figuring out what the biggest improvements to be made to prevent risks to the United States from epidemics. Not necessarily just things that can be a global catastrophe, but natural epidemics and also the potential use of bio weapons or potential biological accidents. So they put out a big report identifying priority areas and their goal was really both to identify priority areas, just difficult because there are so many different types of work that can be done in this field, and to really call attention in the internal DC world, so this is an important topic. We supported their work and that was one of the first grants that we made in the area.
Robert Wiblin: How do you think it went?
Howie Lempel: I haven’t been there for all of the follow-up and it would be great for some folks to, at some point, talk to the new program officer at GMA about it, but our initial question is number one, this type of thing is setting the stage for hopefully having policy changes in the future, and it was largely trying to convene the biodefense community and call attention. So we didn’t really expect policy change to immediately happen, but I think that the initial signs were incredibly successful. So they were able to get a meeting with the vice president; Vice President Joe Biden at the time, and had some follow-up with his staff.
They were able to get several hearings in front of Congress and there was at least some members of Congress who seemed like they might really have the potential to become champions of this cause, and really bring it on as one of their priorities, who seemed to have brought a lot from the hearings, so those seemed to be really good initial signs of success. And OpenPhil actually, since then, has renewed the grant and given them more funding to continue to work and to sort of do follow-up work saying, “We identified these priorities. Has the government made any progress since then?”
Robert Wiblin: Are there any other grants that it would be interesting to talk about?
Howie Lempel: Yes, I think the second one that was really interesting was a grant to an organization called iGEM, which is actually a student competition where undergrad students work on really cutting edge synthetic biology projects, which essentially means that they are combining DNA themselves to modify organisms to do really useful things. So one example of that was neat is that you can modify bacteria and basically make that bacteria into a sensor, so you can have it … An example that was really cool was a project where students created a drug-testing bacteria, so someone could find out whether or not some drug; heroin, was pure, or whether it had been adulterated, by basically having the bacteria react differently to different types of the drug.
And it’s really exciting work, some of the really cutting edge, synthetic biology is happening there and also a lot of those undergrads are going to grow up and be some of the top synthetic biologists down the road. We were really excited about the work that they’re doing, but it’s pretty easy to see how in the long run, this ability for more and more people to be able to modify organisms could also come with safety and security risks. So OpenPhil gave a grant to iGEM’s safety and security team to give them more resources to do things like train those students in how to work safely with the organisms they were working with, because right now the iGEM students are not working with anything particularly dangerous, but those same students down the road could be working with more dangerous organisms.
And then give them resources to teach the students about security culture, and teach them to be guardians of science, and synthetic biology as the field can only really work if you have a culture where everybody realizes that this is a technology that could have huge benefits, could also have huge risks. So the goal of the grant was both to give iGEM resources to have a really good safety and security program, but also to be able to experiment a little bit with that program, because down the road, what we really want is not just this one competition to have a really good safety and security program, but to know in general, what types of things work for creating a culture of safety and security in the DIY bio community in general.
Robert Wiblin: Do you know whether that grant worked out yet?
Howie Lempel: I think we’re still too early to tell. I think we’ll find out down the road.
Robert Wiblin: So we’ve touched on it, but now let’s really dive into the nature of the pandemic risks we face. Why is pandemic preparedness such an important thing to work on? Like possibly the most important thing for people to be working on?
Howie Lempel: Sure. I think the way to start to approach that question is to ask … And the way that OpenPhil originally approached that question was to first ask, why do we care so much about working on reducing global catastrophic risk general? and that ended up being a real priority for Open Philanthropy because we care a lot, both about the well-being of current people, but also about the well-being of people down the road in the future generations, really protecting all of the good things that civilization’s brought for people down the line. So we started out by asking … Right now we have this trajectory where global poverty has been going down for a long period of time.
It seems like the well-being of most people on earth has been getting much better and there’s a lot of hope that in the future that will continue to happen. Are there things that could really destroy that, set us off track? So we went through a process of looking at the main candidates for events that could really disrupt that progress, and if we look at everything from climate change, to pandemics, to risks from emerging technologies to asteroids, war, yes, nuclear conflict, and try to first ask, “What would it take to really get civilization off track?” And that sort of heuristic that we came up with, is we tried to ask, “What are the events that could lead to something like hundreds of millions of deaths in a short period of time?”
When we asked that, and then limit it to areas where there wasn’t enough philanthropy yet and where there were apparent things that philanthropy could really do about it, biosecurity and pandemic preparedness was really towards the top. And I could go through a few reasons why that was the case. When we talk about biosecurity and pandemic preparedness, we usually split it into two categories. One of them is risks from natural pandemics. It could be everything from the flu, to smallpox, to HIV and AIDS. And the other is risks from pandemics that might be caused by humans. So that kind of splits them into two categories. One of them is potentially the use of biological weapons.
A second is the possibility of an outbreak that starts from a lab accident. So somebody doing research, working with potentially dangerous organisms, and accidentally allows some of that to get out and starts an outbreak that way. We looked into both of those as part of the cause area, and natural pandemics, at least in the short run, seem much more likely to occur. We have a long history of natural pandemics occurring. We had several natural pandemics over the last century. Most recently was the flu pandemic in 2009 and new outbreaks are emerging all the time. So if we just want to ask, “What’s the most likely source of a big outbreak over the next several years?” That’s going to be where it comes from.
Then the second question that we asked is, “Could a natural pandemic really get to that level of a global catastrophe?” And that’s a more difficult question for us. We have a lot of examples of outbreaks that were definitely tragedies, where there were thousands of deaths that could have been preventable, but we also have some pretty good evidence of society coming back and being fairly resilient and making it through those events. So we want to ask, “Could a natural pandemic really rise to the level of our sort of threshold of hundreds of millions of deaths?” The main thing that we looked at for evidence was the Spanish flu, which occurred back in 1918. That pandemic killed about 3 to 5% of the world’s population, which if you projected that out to today, ends up at…
Robert Wiblin: … million, 200 million.
Howie Lempel: Yes, exactly … deaths. So that at least gives us a sense that a one-in-100-year-type pandemic might reach that threshold. Those are really difficult questions about if that occurred today, would it be similarly bad? I think it’s hard to know, and having talked to a lot of the experts in the field, opinions really differ. On the one hand, healthcare’s gotten better. On the other hand, we’ve had globalization and outbreaks can spread a lot faster. So when we look at, at least the possibility, it seems possible that you really could have a pandemic of that size from natural causes.
Robert Wiblin: There’s also just a lot more people in some very dense cities, so of course, it’s very difficult to control diseases, right?
Howie Lempel: Yes. That’s a factor too. And then there are phenomena like global warming, which some folks at least think could really increase pandemic risk in the near future as it forces people to migrate a little bit, and move to areas, and come into contact with animals and disease reservoirs that they haven’t touched before.
Robert Wiblin: So, the Spanish flu in 1918, ’19 killed 3 to 5%, which today would be 200 million, 300 million, but that wasn’t even the worst pandemic in history, right? Because it also had the Black Death and smallpox when it got to the Americas. I’ve read stats where as high as 50% of the population have died, or we think historically they died in the very worst cases, when the Black Death came through some parts of Europe. Is that right?
Howie Lempel: Yes, so I’m not sure if we’ve gotten up to 50% of the global population…
Robert Wiblin: Oh no, oh globally, no. It’s locally.
Howie Lempel: Right. There are two questions that you ask when you want to ask how severe a pandemic is. And one of them is how wide it spreads, and the second one is: how likely is someone who catches it is to die? So there are definitely examples of pathogens that killed a much higher proportion of people who were infected, than the Spanish flu did. Black Death is a really good example, and especially the most recent example of one that sort of hit that threshold, but it’s definitely not the only case and importantly, it’s not a theoretical worst-case scenario. So the specific strain of flu that caused the Spanish flu pandemic, it was incredibly contagious. It wasn’t one of the most deadly strains of flu that’s known, so you can at least imagine the possibility of a strain that’s as contagious as the Spanish flu, but that’s closer to having the fatality rate of some of the more dangerous flus out there. And that would be a whole lot worse.
Robert Wiblin: So how many people could die? What are we talking about here? Is billions possible?
Howie Lempel: I think that the answer is it’s possible and there’s no way to rule it out. I wouldn’t say it’s likely that that will happen in the next hundred years, and we don’t have any examples yet of a natural pandemic that has been that severe. But there is nothing ruling it out and we do have this example from only 100 years ago that gets at least within an order of magnitude of that severe, and reason to believe that things could get worse.
Robert Wiblin: Do you want to say what you think the chances are that one of us might die in a global pandemic?
Howie Lempel: I’m not sure if I could get a really good estimate there, and having talked to you almost all of the … A lot of experts in the field, most of them, are not really willing to give an estimate, but something that really struck me is some of Bill Gates’ writing on the topic. He, a couple years ago, put out an article where he said that, “If anything is going to kill more than 10 million people around the world in the next few decades, the most likely thing is a pandemic, either from natural causes or from bioterrorism. So as far as big disasters, that you and me ought to be worried about, I really think it’s right up there.
Robert Wiblin: A lot of people would have seen the film Contagion, which was an attempt to make a scientifically accurate film about how a new disease could spread and the effects it would have, how people would die and social implications that that would have. So in the film A New Disease Moves From Bats to Humans, I think in Hong Kong, from memory. And it spreads around the world and it’s quite contagious and quite virulent, and there’s difficult questions about, “How quickly can we make a vaccine?” And “Who’s going to get access to the vaccine first?” When we’re talking about several percent of the population dying, did you think this one was on point? You’ve seen it, right?
Howie Lempel: Yes I’ve seen it. It’s been a few years so I can’t vouch for all of the details but I can talk to you a little bit … I’ve actually talked to one or two of the experts who consulted on the film, and I can talk a little bit about their view. And I noticed myself talking a lot about having spoken to experts, so I think I should pause really quickly just to clarify that I myself spent a year, year and a half trying to get up to speed on this topic, but I don’t consider myself to be quite an expert in the area, I certainly don’t have a science or medical background.
So, everybody who’s listening should take all these views as my personal views based on a novice trying to get to know the field, and certainly not the views of Open Philanthropy, where I used to work or the views of any specific experts. There’s a lot of disagreement in the field. But getting back to the movie, Contagion, I do think it was a fairly accurate science-based portrayal of the type of really bad scenario that plausibly could happen. And the makers of the film, really wanted it to be sort of a real warning shot. So they wanted it to be accurate enough that it could serve that purpose.
So it’s a Hollywood movie, it means that stuff is dramatized, but they did a really good job of showing a bunch of the really serious problems that could face efforts to deal with a really severe pandemic. In that scenario, you’re going to have a lot of really difficult decisions to make about how to distribute vaccines, how to get the public, when the public is really scared to take the advice of public health officials. All those types of things. And I think the movie did a really good job of showing one by one each set of difficulties that could occur as authorities try to detect and learn about and respond to a really serious outbreak.
Robert Wiblin: So the first time I tried to watch this film I was actually on a plane, and the planes featured in the film is one of the ways of these diseases are spreading, and of course your airports are going to be one of the first places that they show up. And actually, I didn’t manage to get through it because I was starting to get this constant desire to go to the bathroom on the plane and wash my hands. So I set that aside and watched a funny film and then…
Howie Lempel: It was pretty terrifying. It hits the magic point where it both has the plausibility of this is a type of a disaster that actually could happen, and also scary in the way that some of the worst horror films can be.
Robert Wiblin: Yes, it’s too scary to dismiss. So if you’re someone who enjoys I guess documentaries or realistic films about horrible things, then definitely go and check out Contagion. I think it will make it a bit more vivid about what kind of thing is possible that we might end up living through. So what other biological risks that worry you the most? How will a worst-case scenario emerge?
Howie Lempel: It’s a good question. I should clarify that so far we’ve mostly talked about natural pandemics, which are a very serious problem and something I think ought to be taken very seriously, but when we’re talking about biological catastrophes that could really reach the scale where they have a really long-run impact, I think that catastrophes caused by humans actually are an even bigger concern. Over history so far, I think we’ve gotten really lucky that we’ve had fairly few examples of accidents or terrorist incidents or weaponization of diseases but I think that’s going to be harder and harder over time, or at least it might be, to make sure that stays the case.
So we’re seeing over time that it’s becoming easier and easier for more and more people to work with different types of organisms, including some of the worst pathogens out there, and easier for them to modify them. With today’s technology, it’s still incredibly hard to make a biological weapon. It’s still incredibly hard to modify a pathogen to make it worse than what exists in nature, and it’s absolutely possible that that will continue to be the case. But we’ve seen a lot of really surprising progress over time, and it feels like synthetic biology that tries to modify organisms for good reasons and they do good science, but tries to both give scientists the ability to change the characteristics of organisms and also make that technology easier to work with; make it more like a standardized engineering field, and more and more people have access to the technology.
And if that type of technology ends up really successful, I think that’s the type of scenario where you really have to get worried about how you’re going to ensure the safety and security of that field, because pathogens don’t have any inherent desire to hurt as many people as they can. Actually, from an evolutionary perspective, they probably don’t want to kill all of their hosts. So there’s reason to think that there is some sort of limit on how bad a natural pandemic would get, but when you start to think about the possibility of somebody with bad intentions taking a really bad pathogen and making it resistant to the vaccines that we have, things like that, I think that that’s the type of scenario that starts to feel really scary, and that might become more likely over time.
Robert Wiblin: And it’s not only people with malevolent intentions, right? It’s also the military doing this research and then accidentally releasing it, or possibly even intentionally releasing, or North Korea releasing something like this in a conflict. And also there’s people who do this research, that they produce viruses that are resistant to vaccines for research purposes to understand how they could design new vaccines, like how they would respond to this. So what k ind of properties would that virus have. But then if a virus like that escapes the lab, then we could be talking about millions or tens of millions of fatalities.
Howie Lempel: Yes exactly. I think one really good example of this type of research and a really controversial example was a set of experiments from about a decade ago where scientists were working with a strain of flu that is particularly fatal to humans. So it’s a strain of flu that has about a 40 or 50% case fatality rate, which means that about half of the human that get this type of flu die from it. The good thing about this type of flu is that it can’t be passed from humans to humans. So humans can get it from animals. But then once they get it they don’t pass it on, which means that in nature, at least if it doesn’t continue to evolve, it’s pretty limited in terms of its dangerousness.
But then, what these scientists did, is they wanted to learn about, “Could this flu evolve? And what would it take for it to evolve so it did become contagious amongst humans?” So they used biological techniques to get the flu to evolve over and over again until they were working with ferrets, which could be sort of a model of the human respiratory system. So until this flu that was incredibly fatal, could be passed back and forth between the ferrets. We may have learned something from that research. We also ought to be really happy that there was no type of accident because now that would be very scary if it got out.
We don’t know for sure how contagious it would’ve been among humans. It could’ve been contagious just among the ferrets and not among the humans, but it’s an example of the type of research that could create a pathogen that’s actually worse than anything that occurs in nature. I think we ought to be really careful about what types of regulatory systems we have in place, and what types of self-regulatory and government systems we have in place to make sure that we’re being careful when that kind of research is being done.
Robert Wiblin: So if we were unlucky and that virus escaped the lab, and we’re also unlucky and it turns out that it is contagious between humans and the case fatality rate holds up, we could be talking about a billion fatalities, like really serious social dislocation. This would be a catastrophe, right?
Howie Lempel: Yes.
Robert Wiblin: It’s really one of the worst catastrophes in human history.
Howie Lempel: Yes that’s right. So one way to think about that again, is you can think about the Spanish flu, which is one of the more contagious strains of flu that exist, and something like half the global population caught that flu. If they were to somehow take the flu that has a 40 or 50% case fatality rate and make it that contagious, which it’s not likely that has happened yet, but if it were to happen and it were to get out you can imagine something like a quarter of the world population being killed. That’s a worst case scenario but it’s pretty scary to know that something like that would even be on the table.
Robert Wiblin: There’s a game, Pandemic I think, where the goal of the player is to kill as many people as possible. They’ll try to drive the human species extinct I think. It seems like people in that game always survive in Madagascar. That’s like a famous … ‘Cause Madagascar only has one port and it closes it right away. I guess that there would always be people in Antarctica or on ships and so on, who would avoid this kind of thing. So it’s not really plausible that everyone could die from this, but like a quarter, you’re saying, is imaginable.
Howie Lempel: Yes, from that type of experiment in a real worst-case scenario, yes I think that’s about right. People have certainly come up with some scenarios that are really science-fiction today but that if you are really devious and lucky and talented, could be even worse. So not that we should always be open to that possibility, but I’ve raised a basic point that it’s very unlikely that anything will occur, that everyone in the whole world would catch, and that nobody would be resistant to. But you’re going to have to ask all the questions about what type of disruption do we have to governance and society, even from the smaller incidents.
Robert Wiblin: Right. So did you or OpenPhil form a view on whether there’s a risk of widespread social collapse if something like a billion people would die in a pandemic? Because you mentioned people make this argument with climate change, with war or nuclear war, so initially it will be bad, but then as all of our systems of trade fall apart, as borders are closed, as people panic, we’re going to have declines in the quality of governance and people will turn on one another. The legal system might break down and so things will move from bad to very bad. Is that something you have a view on?
Howie Lempel: Yes. It’s a really hard question and it’s one of those questions where I think we don’t really know unless it happens. We don’t have any case studies to look back on, that we can say are like a real analogy that’s happening and go one way or the other. I definitely can’t speak for OpenPhil but my own view is that … It’s absolutely plausible that society would come back from an event like that. We have had some real serious disasters that society did come back from. The Spanish flu and World War I, World War II, all sorts of pretty good examples of the type of event that you might have expected to really lead to major decline in governance, and that we seem to have come back from, but this did not lead to something like a billion deaths.
The world changes over time, and also that’s only two examples. I think personally, we really want to avoid ever taking that type of risk. In the whole history of humankind, it’s a pretty short period where we’ve had things like liberal democracy and the types of institutions that support poverty reduction and scientific progress. This does seem like the type of thing that’s potentially major disruption, and if this does occur, you’re going to have governments making a lot of really tough decisions about things like how to allocate vaccines, whether or not…
Robert Wiblin: Who lives and who dies.
Howie Lempel: … who lives and who dies. And what that does to this sort of fragile trust that people already have in a lot of governments, I think is a really, really open question. So I think it’s pretty important that the world does anything possible to avoid having to learn that answer.
Robert Wiblin: Yes I guess some other differences between World War II and the pandemic today are that an international conflict or a war like that produces intense social solidarity within each country, and it’s not clear that that carries over to a pandemic where you don’t have another human enemy that you are rallying against. Although I guess it could be better in some other ways. And of course, just busy. A lot more international trade now I think, and a lot more complicated technology such that we don’t know what would happen if international trade was cut off and suddenly people can’t get the supplies they need to keep electronics working and things like that.
In another sense where we’re more robust now because we’re quite a lot richer than people were then. So even if our incomes halved by this kind of disaster, we’re probably not going to be starving, or at least unless the food supply is targeted specifically or experiences disruptions. So in that sense we’re more robust, but at the same time, because our technology is so internationalized and so sophisticated, it’s easy to see that we might not be able to keep it running. If a lot of nuclear experts die of the disease how do we keep the nuclear power plants running?
Howie Lempel: Yup. I think that’s absolutely, those are the right considerations for sure.
Robert Wiblin: So we’ve talked about the plague and about Spanish flu and smallpox, but there’s other historical analogies and some other recent ones that we might want to think about if we’re looking at what’s the distribution of how contagious or how virulent new diseases are. Just recently we’ve had Zika, so it was just carried by mosquitoes and usually just produces flu-like symptoms, but also sometimes produces paralysis we think in a small fraction of cases of temporary paralysis, and also produces deformations in the children of pregnant women. That’s one that we just couldn’t control. I guess it was just too contagious for any of the … or before we recognized what was happening it was already too widespread.
I guess we’ve also got Ebola, which is extremely virulent in that it kills something like half of people who get it, or at least half of people who’ve gotten it in Africa. But it’s not that contagious because it has to be passed through bodily fluids, right? So it’s not very good at spreading, so the recent outbreak was by far the worst case, and even then, by improving burial methods mostly we were able to get it back under control. But it’s an example of something that we knew about, but in fragile states where the healthcare system is very poor, we’re not able to prevent every outbreak. Sometimes it does get out of control and then we have a difficult fight on our hands to stop it from spreading.
Then there’s other flu outbreaks; we had the Swine flu where there was an effort to try to quarantine it, contain the virus, but again, just the public health systems, at least in Mexico and the other countries it got to by the time we realized what was going on, were just not up to the challenge of containing it. And that’s the virus was just so contagious that it was never going to be realistic to cordon it off. Then we’ve got other cases like SARS and MERS; these are respiratory syndromes. SARS we managed to contain in 2003 with only I think a couple of hundred fatalities, and maybe only a few thousand cases from memory.
And that I think that it was in China and Hong Kong and Singapore, were the main countries. I think it probably was brought under control just because they were extremely vigilant and actually very good at following up on cases, so they were able to find everyone who’d been exposed, and even though it did seem to spread very well through hospitals, they managed to bring it under control. So that’s a good case for humanity. Hopefully we’ll be able to catch things early enough and be diligent enough, but not every country is quite as organized as Singapore. Are there any others that we should think about? Are there cases that we can learn from recently?
Howie Lempel: I think you covered the most important ones, and there’s some lessons to take away from that. One thing that someone might think is we have thousands and thousands of years of human history, and humans have been pretty resilient. No, we haven’t had a pandemic that’s really wiped out civilization yet, so someone might use that as evidence to say, “Hey, we’ve come into contact with most of the pathogens out there, so it seems pretty unlikely that there’s some unknown one that really could cause us a type of damage. And I think that some of the new emerging diseases that you mentioned are pretty good evidence that we shouldn’t be so sure about that.
So SARS and MERS and ZIKA and HIV/AIDS are all examples of diseases that newly emerged, as far as we know, over the last hundred years or even more recently. So they’ll give us reason to think that there still are pathogens out there whose effects we don’t really know about yet, so that’s one implication of those historical cases. A second one that we’ve seen is, as you mentioned, we have some pretty good cases where countries like Singapore and Hong Kong have shown how you really can limit the spread of some pretty serious diseases if you have a really good control system in place. So I think that that’s some good news.
On the other hand, those weren’t nearly as contagious as something like, particularly contagious flu like a … And then Ebola, it gives us some evidence of some of the limitations in poorer countries with health systems that really don’t have the resources to tackle this type of outbreak, how long it can take to get an outbreak under control, even for a pathogen that doesn’t spread that quickly and that would be fairly easy to control in the developed world. So I think that that is a really good warning scenario. Ebola, fortunately, doesn’t spread that quickly so it’s really not the type of pathogen that could cause a global pandemic, because once it gets to the developed world, if somebody is really isolated, if a hospital is using all of the appropriate procedures and has contemporary top technology, it’s much, much, less likely for them to pass it on.
But we saw how much even that was able to spread in West Africa, so we have to ask if it had been a really dangerous flu instead, how fast would it have spread? And how many people would have it by the time it started spreading outside of the area where it originally started. If it took us as long as it did to respond to something like Ebola and get it under control, I think it’s a real warning shot for what could happen with something even scarier.
Robert Wiblin: Yes. Sometimes when I raise this issue with people who don’t know a whole lot about pandemic risks, they say, “I think that the public health people will have it under control. They’ll be able to contain the disease.” But we basically know that that’s not the case because we have all of these instances where there were attempts to control a disease and it didn’t work out because we’re just not good enough at doing that. It’s a very difficult task. And even in countries that have very good healthcare systems, which isn’t everywhere, if you don’t catch it early enough, or if it’s very contagious, or if you get unlucky and one person exposes the disease to many people, perhaps in a hospital, then it could just spread like wildfire, basically.
Howie Lempel: Yes, one of the big lessons from the folks who study these types of emerging outbreaks is the importance of early detection, because a lot of the strategies that we have for response, depend on the response happening when not that many people are sick yet. So one of the most effective techniques that we use is called contact tracing, where you go to everybody who’s gotten the disease and you track down every single person they’ve gotten into contact with, and you ask all of them to maybe go on preemptive drugs or to isolate themselves until they know that they’re not sick. That’s viable if you start without that many people who have the disease. Once it’s gotten to a certain scale, you just can’t imagine having enough public authorities to do that, so early detection is really key. And something we learned from Ebola, is that we don’t really have the global systems in place to do that.
One thing that we really saw is the limitations of even our planning for what to do in a case of a … In the scheme of things, some are limited outbreak. A lot of people assume that the WHO is the global authority who ought to be in charge of this type of outbreak, and one thing we definitely learned from Ebola is that they just don’t have the resources to do this type of thing. They can provide advice and technical support to the governments in the countries affected, but there’s no huge WHO strike team that can just zoom in and mobilize as soon as there’s a outbreak. And it really took countries like the United States and the Centers for Disease Control there, and the US military, to show up and voluntarily come and work on disease control. That takes a whole bunch of time to mobilize because there’s no default automatic plan for that to happen.
Robert Wiblin: So we’ll come back to that in a minute, but first I wanted to ask you, how do you think the risks here are affected by things like sloppy research security or by the existence of factory farming, which creates lots of human/animal contact or people eating wild animals, bushmeat in some countries, which then is another route by which diseases can spread from animals, and especially animals that humans have been exposed to that much into humans. Or perhaps the overprescription of antibiotics. Are there some large contributing factors here that maybe we should be targeting?
Howie Lempel: Yes, so I think that all the factors that you mentioned are important factors. They all fall under … When we think about interventions to reduce these risks, we talk about preventing outbreaks, detecting the ones that occur and responding to them, and those are all in the prevention bucket, in preventing the initial spread. Some of them, I think, are a bigger deal than others. We talked about how natural pandemics are the bigger risk today, but there might be even higher magnitude risks down the road if biological technology really gets more powerful. So today, I think if there’s going to be this type of pandemic that really could cause a global catastrophe, it’s almost certainly going to be from an emerging disease, from a disease that we don’t have that much experience with, so it might be a new strain of flu, or it might be something that we don’t even know much about.
Those tend to come from zoonotic areas. So it tends to come from diseases that lived in an animal population for a long time, and then spreads from animals to humans, and turns out to be really deadly in humans. So a bunch of things that we want to look at there are areas where there’s a lot of contact between humans and animals. It’s one reason why there’s been a lot of focus in the flu community on areas of Asia that do chicken farming, and where there is a lot of contact between birds and humans. So I think that having really safe practices around how animals and humans interact is pretty important in that respect.
Down the road, if we end up in a world where there are bigger risks from biological technology, I think that’s where lab safety practices are going to be really important. It’s the type of thing that I think is really frustrating to focus a lot on. If you’re a lab scientist, every single day your priority is to make progress in your research, and a lot of the safety measures I think feel like checking off a box, but you’re not only risking your own safety, if you get something that’s really contagious you could be risking the public safety too. So I think that that’s going to be a really important area.
And then another really important area is going to be thinking about how to prevent the spread of technologies that could be used for ill, and we can draw an analogy to the nuclear nonproliferation world, where we have a lot of rules about what countries are allowed to have nuclear weapons and how many. We sort of have a somewhat similar regime right now about biological weapons, but most of the rules cover a certain list of pathogens that you’re not allowed to take across borders, and that doesn’t work anymore. If we’re in a world where folks can create totally new unconventional organisms that aren’t going to be on the list, or if they could create something that they don’t even know is going to be dangerous, or they might not even be moving an organism from one place to another.
If synthetic biology is really successful and you can create a new organism from scratch, then just having the information of the sequence for this pathogen might be enough to create something really dangerous. So I think there has to be a lot of thought put into what nonproliferation means and looks like in a world where just searching people’s bags for vials that look dangerous in the airport really becomes kind of irrelevant.
Robert Wiblin: So during the Cold War, I think the major powers spent quite a lot of money on these biological warfare programs trying to come up with pathogens that could be used or that they would claim just for the purposes of defending themselves against other people who might develop them. But we’ve never ended up using them. As far as I know, they haven’t really been used in a war. Is it just that they’re not really practical to use because they’ll come back and bite you in the ass, right? If these things spread, then they’re going to end up infecting your own soldiers
Howie Lempel: I think that there are a few reasons why they haven’t been used, almost never been used so far. One thing that’s important to clarify is that my impression at least, is that when countries were researching biological weapons, which is now banned by the Biological Weapons Convention, but previously wasn’t, and we’ve learned that even after it had been banned, the USSR had a major biological weapons research program for a long time in secret. But the weapons that they were mostly working on, weren’t the type of things that could cause the type of catastrophe that we’re talking about.
Robert Wiblin: It’s localized.
Howie Lempel: Yes. So the most common things that are talked about as biological weapons first are things like anthrax, which we have seen examples of being used, but fortunately it’s the type of thing that’s in some ways a little bit more similar to a conventional weapon, in that once someone is harmed by it, it can’t spread. So you can imagine a really terrible tragedy that occurs because of the use of anthrax, but it’s really hard to imagine something that’s globalized and really has an effect on the long-run future, because somebody who gets anthrax can’t then spread it on to the next person.
Robert Wiblin: So it’s more like chemical warfare in that respect?
Howie Lempel: Yes, it’s more similar to chemical warfare in that respect. And the things that we might be a little bit more worried about are the use of something like smallpox or the flu, where you could infect your enemies, soldiers or civilians, and then they would pass it on, and you really could see a global impact. And as you pointed out, there are several reasons why no country has done that so far. One of the main ones is that there’s no way to stop it from then coming back and infecting your own side. So there are some really strong incentives for people not to use that type of weapon. It’s a little hard to even imagine the person for whom it would be a rational decision, what types of goals you could have that would make it make sense.
Robert Wiblin: I guess North Korea using it for blackmail or something like that?
Howie Lempel: Yes, I think that that’s one example. We do have a few examples over history of suicide cults who just had a worldview where they just thought it would be good to kill as many people as possible. Aum Shinrikyo, in Japan in the 90s was one example that actually did try to have a biological weapons program. They weren’t successful but that’s another example of the type of ideology that could lead you to do this thing. And so far, we’ve been fortunate in that the technology to weaponize diseases has been difficult enough to work with that you really needed to be at the scale of a country government, to use it successfully. And it’s pretty hard to imagine getting enough people to buy into this idea to want to do something like that. The danger is that down the road if it becomes possible for a few individuals, and maybe not even individuals with a PhD in biology, but people with some amount of background are also able to work with these types of pathogens. That’s where we might become a lot more concerned.
Robert Wiblin: So let’s turn now to thinking about what’s already being done. We touched on this a bit earlier, but when a pandemic starts who exactly is responding, and what are they going to try to control it?
Howie Lempel: So something to start with is … Once a pandemic starts there’s two phases. One of them is the detection phase, and the next one is the response phase. At the detection phase, where the relevant authorities are first trying to figure out if a outbreak actually exists, and then figure out what sort of outbreak is this, how serious is it, what type of measures do we need to take to put in place, it’s mostly going to be done depending on where exactly it occurs by local individual doctors and hospitals, and then country governments, and then possibly nonprofits and NGOs. So it’s important to find out that nobody knows when a pandemic starts. So a pandemic is a outbreak that eventually becomes global and is a certain level of severity, so when you first notice … The first time that someone shows up to a hospital sick with a symptom that will become a pandemic, nobody has any way to know that it’s that severe.
They’ll likely show up to a hospital and they’ll have flu-like symptoms or something like that, and there’s a question of how long it will take before anybody notices that something unusual will happen. So the term of art for that process of noticing that something unusual has happened that requires a response is called “disease surveillance.” And that works differently in different countries, but the general idea is that there are few ways that a potential pandemic might be detected. One of them might be with real sort of formal diagnostics, so if somebody might come to a hospital and if they have Ebola symptoms and it’s pretty far into the direction of the disease … Diseases like Ebola look pretty similar to each other so it’s at least possible that a doctor will notice-
Robert Wiblin: Hemorrhagic fever, that’s right?
Howie Lempel: Yes, so there’s a set of hemorrhagic fevers, they all look pretty similar to each other, but at least far enough into the disease look reasonably distinct from other diseases so especially if you’re in an area where doctors have seen Ebola cases before, a doctor might notice, then there are specific diagnostic tests for detecting whether or not somebody has Ebola, so a doctor will have to … might either already have those diagnostics or might have to get the diagnostics, and you might get tested and if there is an Ebola case somewhere, there’s at least supposed to be a reporting system where the doctor will probably report it to the ministry of health, who then is supposed to report it to the WHO, and then there’s some type of global knowledge of the fact that there’s been an outbreak of a disease that could potentially cause a public health emergency.
That’s sort of a … in some ways, it’s a tragedy but it’s also in some ways the best-case scenario, because it’s the disease that looks reasonably distinct. The more likely scenario and the scarier scenario, is that somebody gets a really dangerous disease, but that it looks like a disease that is endemic to the area; a disease that people get in the area every day.
Robert Wiblin: It looks like malaria.
Howie Lempel: Exactly. So that’s a really good example, is that one of the main symptoms that someone who has a really dangerous flu might have is a high fever. That could also be malaria, it could be measles. If somebody shows up to a hospital with a high fever, it’s not a all-clear that anybody would know what the person has. They might just assume that it’s one of the many people who has something like malaria.
Robert Wiblin: And they might not even test. They’re not going to be asking the question, because you can’t test everyone who comes in with a high fever for everything that they might have.
Howie Lempel: Exactly. So one limitation, a major limitation of most of the diagnostics that are currently in use, is that we don’t have very successful broad-spectrum diagnostics, which means diagnostics where you can take one sample from somebody and just ask what is this person infected with, and instead, the way that most diagnostics work is you get diagnosed for a specific pathogen. The doctor essentially has to take an educated guess at what the patient might have, and gets a yes or no answer, which means that if somebody shows up and their only symptom is a fever, and the doctor isn’t yet aware that there’s some outbreak taking place, it’s really tough for anybody to diagnose that there’s anything out of the ordinary going on.
It might not become apparent until at a certain point, in a certain location, there are many, many more people coming to the hospital than usual. And that might be the first time that anybody realizes, “Oh, this isn’t our normal level of background disease but something really out of the ordinary is happening.”
Robert Wiblin: So they’re going to have to test them for the first thing they think they have, and then the second thing, and then the third thing, and then they might give up, and maybe they’ve gotten better or died by that point.
Howie Lempel: Exactly. And because that’s how the system works, for a lot of diseases people won’t get a diagnostic at all. So if you’re in an area where malaria is pretty prevalent and someone shows up with a fever and malaria-like symptoms, often the best practice is just to give the person malaria drugs and send them home, and they don’t even bother to get a diagnostic in the first place. So in that type of case, it really takes a noticeable number of people infected before anybody would realize that something’s amiss.
Robert Wiblin: So you mentioned that the World Health Organization automatically gets notified, but what do they do? You’re saying they don’t have that many resources to act. Do they just tell all the governments that there’s a problem?
Howie Lempel: Yes, there are two really important issues there. One of them is that there’s a set of guidelines called the International Health Regulations that govern what countries are supposed to do when they learn that there’s been an outbreak of the type of disease that could cause international concern. So it doesn’t even necessarily have to be something that could rise to the level of a pandemic, but the type of thing that countries around them ought to know about. One aspect of that is that they’re supposed to have enough surveillance systems in place and response systems in place that they are likely to notice if it happens. The second aspect is that they are required to report it to the WHO.
Very few countries are actually in full compliance with the International Health Regulations for a bunch of reasons, but one of the main ones is that it’s just really expensive and really hard to get all the way up to there if you’re a country that might not have a lot of resources, and might have on a day-to-day level, might have a lot higher mortality rates from the types of diseases that are endemic, that people are getting all the time but that aren’t likely to spread abroad, so they might be more concerned with those types of issues. So countries often aren’t in compliance with the IHRs and some might not know this. And then even if they do know this, a lot of countries really resist telling the WHO about the problem.
There’s a lot of concern that knowledge of an outbreak will lead to things like a stigmatization of people from that country or boycotts and immigration barriers and that country really being closed off and taking a big economic hit. So that’s a second major issue, is that even once countries discover that there’s an outbreak giving them the right incentives so that they actually report it is a tough problem. And then if they do report it to the WHO, as we talked about, we would like to live in a world where the WHO then has a lot of resources to deal with it. That’s not really the world that we live in. They do have a outbreak alert and response team. It has very, very few people.
There are a bunch of proposals on the table, especially as a response to Ebola to really beef that up. But so far that hasn’t happened. So what the WHO does is make it public that this is happening. They’ll provide some types of advice and technical support to the ministry of health in the country that’s affected, and they might serve sort of a coordinating role as they try to get other countries to cooperate in addressing the outbreak. So if the outbreak is happening in a rich country, then you might see the rich country mostly dealing with it on its own. If the outbreak is happening in a poorer country or a country with a less well-developed outbreak response system, then you’re probably going to need doctors from outside of that country and epidemiologists to come in and provide assistance.
The WHO might be able to coordinate that, but that’s going to be each donor country’s individual decision about whether or not they want to provide assistance and what type of assistance they want to provide. There’s no automatic system for that to happen immediately. What ends up usually happening because of that, is that the first responders are sometimes organizations; like Doctors Without Borders is a really good example, so NGOs that already have doctors that are experts in the country, just showing up and doing whatever they can do. And they’re often experts in crisis response, but aren’t in any formal way able to bring in the types of resources that a large country government could bring in instead.
You would like in an ideal world to have a coordinated global system, where it’s very clear who’s responsible for making a plan, who’s responsible for providing resources, who’s responsible for scaling up resources if it’s needed it be, but instead you have a much more fractured ad hoc system, where the country that’s affected will have their ministry of health doing what they can do, and then you might have some nonprofits, each doing what they can do but without any already built-in communication and coordination system. And then eventually, you might have donor governments and philanthropists as well.
Robert Wiblin: So there’s a lot of problems here, it sounds like. So even when the WHO is alerted, hopefully ultimately they’re alerted to the fact that there’s a new disease spreading, there’s no group of people to swoop in and solve the problem. They’ve got only a handful of people that they can afford to pay to go in and try to intervene if this is happening in a country without a great health system. So they have to wait for richer donor countries to pony up some money, which could take weeks or months. And also because there’s no way of fairly distributing the costs among those countries. I imagined they’re inclined to wait and hope that another country will pony up the money, and they didn’t have to spend it themselves. Is that right?
Howie Lempel: Yes, that’s exactly right.
Robert Wiblin: And by the time you get to the stage where they’ve got the money, they’ve convinced the donor countries to give, and now they’re starting to coordinate it, it could just be all too late.
Howie Lempel: Yes, so I think that those are … All of these stages of response, and at each stage I think you’ll find major obstacles and you identified several. So the next obstacle that often comes along in this realm of WHO coordination, is that once you do start to have a response, one of the first things that you want to do, is if it’s an emerging disease that it doesn’t have necessarily a highly effective vaccine yet, then you immediately want to get a sample of the pathogen, sequence it, and get people working on treatments and vaccines. And there are a lot of issues there, where we don’t have a very good system established for how to share all of the data that is collected as part of this. So who owns the data when it’s eventually sequenced? If a vaccine is created, who owns that vaccine? Often, those types of things are being worked out on the fly, and you have all these international negotiations that are happening in the midst of a crisis.
Robert Wiblin: Right. So charities are pitching and it seems a bit crazy that the planet relies on private charities to do this kind of disease control but some charities will do that. Are they potentially a good group to get involved with?
Howie Lempel: Yes, so I will first caveat this by saying it’s a really big field pandemic preparedness, and I’m definitely not an expert in every area. This is an area where I wish I was more expert than I am. I think that a lot of the organizations who do this rapid response are incredibly valuable, and I don’t know about their work firsthand but I’ve talked to a lot of people about the great work that these organizations do, especially Doctors Without Borders in particular. That said, as you pointed out, I think that the eventual system that we want to land on is not whatever doctors happen to be there holding the fort until the real response happens.
And so, because in the long run I think we really want some type of more coordinated planned out system, and because to the extent that we don’t have that system, I think in a worst-case scenario it really might be there’s too little that those types of doctors can do. So my instinct is that, that’s not the first place I would work on if I wanted to really reduce risks from pandemics. I do think it might be an incredible learning opportunity, and opportunity to really get to know the field, and I think it’s hard to advocate for policy change is areas that you haven’t seen up close, but in the long run I think the type of change that we need to see.
And I think organizations like Doctors Without Borders are often the first ones to say this, is that they will be the band aid, but they are very vocal about the fact that they do not think that they ought to be the ones who are the band aid. So think the things that would be in the long run more effective, are things like pushing for the WHO to have the resources to do this thing, or if it can’t be the WHO, pushing for the creation of a new international organization to do it. Or if not that, pushing for rich country governments to provide this type of response, and then finds more leverage points.
So it might be that instead of focusing on the response after the outbreak has already happened, to focus on ways to detect outbreaks sooner or focus on ways to prevent them from starting in the first place. The other thing about that type of work that might make it a little bit less neglected in some of the areas, is that the type of immediate response by NGO doctors on the ground, that you see happen for a potential pandemic, I think is going to be the same type of person that you see responding to more frequent outbreaks. So that means that there’s a little bit more attention to that problem, than the problem of how someone would respond specifically to the types of scenarios that we don’t see that often, but that could be something like another Spanish flu.
Robert Wiblin: To the big one.
Howie Lempel: Yes.
Robert Wiblin: So we’ll come back to what kind of reforms we want to see in a minute. But how long would it take to start making a vaccine for a new disease, if we could develop one at all? Are we talking weeks, or months, or years?
Howie Lempel: I think that the best answer is that we’re not totally sure. It depends a lot on the specific pathogen, it depends on our standards for how good the vaccine has to be, it depends on their regulations, a place in a specific country, and it depends on how much of a priority the global community puts on making the vaccine. But to get the sense, one extreme is that people have been trying really hard to make a vaccine for HIV/AIDS for decades and still have not been able to develop one. It’s a virus that for various reasons is particularly difficult to make a vaccine for …
Robert Wiblin: Because it’s constantly evolving.
Howie Lempel: Yes, it mutates a lot. So that’s an example where you can have decades of effort and still not have a vaccine. Every year, for the seasonal flu, doctors develop a new vaccine that and a lot of people in the developed world get every year, they have to guess far in advance what strains of flu are going to be the next seasonal flu because it takes months to develop the vaccine and then manufacturer enough of them to have it at scale. So I think we’re really, in the most likely scenarios, talking about a few months to develop a vaccine that works and a few months to then manufacture a lot of it, and then you have lots of questions about how much do you want to test it out if it’s really new before you use it at scale and all those types of things. But even-
Robert Wiblin: If people are falling down in the streets you might want to scrimp on these safety testing. It’s just not safe not to release it.
Howie Lempel: That’s … I think a really difficult question, and I think in a real worst-case scenario, ideally you would want to do that, but you have a lot of risks especially in places where people don’t trust the government that much, where if you have a few cases where somebody is harmed by their vaccine, you could really see people stop trusting the public health authorities and…
Robert Wiblin: And then even if they produce a safer vaccine later…
Howie Lempel: Yes, exactly. So that’s a big risk. You also have a problem where ideally you want the vaccine to be rolled out in a way where you’re tracking results, so you can also be learning over time about the effectiveness of the vaccine, but there are all kinds of issues with the regulations and ethics around doing that. And then even if there’s consensus around maybe reducing the amount of safety testing because pathogens is that dangerous, you still need to have a legal process to make that happen, and often the regulations just aren’t there if a country hasn’t thought in advance about, “What would we do in this type of crisis?” So I think one thing that’s really important, is every country ought to have a plan for what they would do if this were to happen, and a lot of countries aren’t there yet.
Robert Wiblin: I’m sure that we can trust Congress to make scientifically grounded decisions on the fly about these difficult public policy issues.
Howie Lempel: Yes they have a pretty good track record of that [laughter 01:13:54].
Something that actually was really disillusioning for me, was Congress’s lack of response to the Zika virus, and it’s coming just on the tail of Ebola. So at a time where there really was a lot of public attention on dangers from outbreaks, and it was months and months where the CDC was begging for more funding to work on learning about Zika, preventing it from spreading to the United States, and Congress basically kept asking, “Why can’t you take the money that we already allocated for Ebola follow-up and use that on Zika instead?” So I think that that we shouldn’t be too confident that lawmakers will be able to handle this type of thing on the fly. On the other hand, Zika is not a particularly deadly disease, and you might see more of an attitude of crisis management if we really had something a lot more dangerous.
Robert Wiblin: So it sounds like in very poor countries, the response is going to be very unsatisfactory, and that the international coordination mechanisms are also really not up to the task. But what about the government in the US overall? Do you think it’s doing a reasonable amount to protect us from this kind of threats? I know we have the Centers for Disease Control.
Howie Lempel: Yes, so in some ways yes and in some ways no. The United States spends a really large proportion of the global resources going into these types of issues, and I think that that’s really impressive and really important, and the United States has a relatively successful public health system for certain types of diseases. Something like Ebola, there’s much less chance of spreading to a US hospital, which has even basic things like personal protective equipment like the gloves and masks that nurses and doctors are supposed to be using can run out in poor countries. So there are a lot of advantages in the US.
That said, I think that there’s still, even in wealthy countries like the United States, a whole bunch of gaps in the systems that we have in place. Some of them are gaps in the resources that we dedicate to this type of thing, so I think it’s really important to see the US government dedicate more resources to fighting assistance to countries with fewer resources, so that they detect outbreaks earlier, which I think would also be helpful for countries like the United States. Because diseases really don’t respect borders and can spread quickly. Another issue is that it’s just a really difficult problem to make all of the local healthcare providers around the country know how to respond to some disease they’ve never treated before.
You saw that in the Ebola context, where there really was a lot of panic by our local healthcare providers who didn’t necessarily know, “What type of personal protective equipment do I have to use so that as a nurse I don’t get sick?” Like, “Which people do I have to isolate?” All those types of things. And there was a difficulty in responding in a crisis. Another big problem is that even though the US does have the CDC, there’s a lot of ambiguity still over in the case of a really severe outbreak, who exactly is in charge. So there’s the CDC, there’s other parts of Health and Human Services, there’s the White House, which in the case of Ebola, set up a special White House Ebola Czar.
If there were any risk that something might be an intentional release of a biological weapon, then you’d have law enforcement involved. There’s state and local actors, there’s the NIH that heads up a lot of the research, but there’s also parts of the Health And Human Services like BARDA that also are working on research, so there’s a lot of different people, all of whom are in charge of a chunk of the response, and no person who’s the one person who’s totally accountable. So I think the best place right now to go if you want to see a list of the many ways in which the US government could improve its responses, is really the report that Open Philanthropy funded that was made by the Blue Ribbon Panel Project on biodefense. And they were able to identify a lot of gaps where US policy could really improve.
Robert Wiblin: And you haven’t even mentioned the military yet, probably could get involved, especially if there was a need to move people overseas to areas where a disease was spreading. I think that they automatically had to get involved in the Ebola case because no one else would fly there or no one else had the capacity to bring in the people and equipment, right?
Howie Lempel: Exactly. And the military also is the one agency that’s focused the most on defense against biological weapons so if the pathogen that was getting passed around was the type of pathogen that people had worried might be used as a biological weapon, often a lot of the experts will actually be out of the Department of Defense. They also just have much more logistics capacity so if you need to do something like set up tons of mobile hospitals they’re the ones who are able to do that, and there’s often some tension between the health side and the defense side. I think there could really be more of a process for facilitating communication across those cultures. So I think that that coordination role is really a gap.
And then something to also add that’s a particular gap in places like the United States, is because of just how the political system works, I think that there’s a temptation to always be preparing for a crisis that looks exactly like the most recent one, instead of thinking towards the future. Part of that’s like a natural human tendency and part of that is because of just the incentives facing politicians, where if Health And Human Services is putting a lot of research and resources into researching a vaccine for a pathogen that would be really awful if it spread, but it’s very unlikely to spread, every year that Congress asks, “What were our results? How many lives did this save?”
Until the one time where it really matters, t answer is going to be, “it didn’t help.” So there’s a lot of pressure on them to show results, which means working on the more frequent epidemics or the ones that might not be as severe, so I think that there’s a real need for just to in any way possible subsidize or advocate for work that would specifically address the types of things that would be real worse-case scenarios.
Robert Wiblin: So I’ve read some books about this general topic lately and I’ll stick some links up to them in the notes on the episode. There was a particularly good one by Laurie Garrett about the Ebola outbreak and how we responded and the ways in which it was really, really not sufficient. So let’s focus now on what can be done to make pandemics less of a threat to humanity. We already touched on this a bit but what kind of people do you know work in the area and what are they doing? Even the ones OpenPhil hasn’t made rounds to.
Howie Lempel: Yes so there are a whole set of areas that I think are really important. One way to organize them, which I’ve referred to a few times, is prevention, detection and response. So I can talk about some things that strike me as really important in each of those areas. In the prevention area, there is preventing the occurrence of an outbreak of a natural disease, and I think that’s pretty tough but there’s some really interesting work there, particularly on trying to surveil animal populations. So learn about what diseases are already floating around among animals, and whether or not any of them are reasonably close to the type of disease that could cause potentially a really severe pandemic among humans.
I think that that’s really important, and if you know the answer to that, then you can also take steps for prevention like focusing particularly on limiting contact with animals in certain populations, or if you have to call certain populations of animals … If you want to prioritize preparing by stockpiling certain vaccines, all those types of things, require you to do that type of preparedness in advance. So that’s one area, and a lot of people are working on that type of thing. And then I think maybe an even more neglected area of prevention that I think also is neglected because it’s focused in particular on things that aren’t a risk today, but that we might need to plan for down the road, is thinking about how policy might have to change if biotechnology really advances really quickly, and what we could do to prevent an outbreak in that world.
So there are things in that area like thinking about what type of regulations we would want to have on the use of desktop synthesizers, if it became possible to synthesize a virus from scratch. Or today, we have a lot of DNA synthesis companies. They are companies you can basically call up and say, “Here’s a sequence. I want you to synthesize some DNA with this sequence,” and you can order it. There are still technological limitations to how complicated of an organism you can order and those firms are supposed to screen … There’s an agreement to screen the DNA before they send it to you to make sure that you’re not ordering anything unsafe…
Robert Wiblin: You don’t want people ordering smallpox.
Howie Lempel: Exactly. There’s not yet a ton of information about how accurate those screening processes are. Do we know if all the firms are using them? And especially, there’s more information about firms in the United States than there is abroad, but as biotechnology becomes accessible to more and more countries, which is a good thing, it let’s them have really important medical industries, that we really want some types of international agreements on what does screening for this look like? Are you only screening for known threats? Or you going to try to identify certain characteristics that might not occur in any natural pathogens, but that could make a pathogen really dangerous? If you do that, do you want that information out there about what types of sequences you’re banned from synthesizing? Maybe not, if that is creating a recipe for … so there are a lot of difficult policy questions.
Robert Wiblin: It would also allow people to evade it if they knew what the rules were.
Howie Lempel: Exactly.
Robert Wiblin: They could just do the thing that didn’t quite trigger the alarm.
Howie Lempel: And I think there’s consensus among most people in the field that these are difficult important questions. There’s also a consensus that we don’t want to panic because the technology isn’t there yet, but I think something that would be really scary is if we first start to address these types of policy issues after the technology has already developed, and there have been some people doing really good work on this type of stuff. The Veterinary Institute put out maybe five or six years ago a really good piece on the governance of synthetic biology that talked about new types of screening technology. But that was five years ago, technology moves really fast.
I think we’d really love to see updates on that kind of thing. So in this area, there’s diplomacy that needs to be done in getting countries to agree on international standards. There is science that needs to be done and computer science, in like … How do you set up these screening technologies? There’s a lot of work there, in thinking about what does nonproliferation look like in this area. And then similarly, that’s all sort of addressing who gets to use this technology and how do we enforce that? There are also questions about safety and what types of requirements do we want to have on labs or on individuals who are working with dangerous pathogens.
I think that there’s a lot of opportunities for research there on both … Are there better safety techniques that could be used? Are there ways to specifically engineer an organism so it couldn’t survive in the wild, if you’re working with something that’s dangerous? So there’s a lot of science there. There’s lots of engineering questions about if people are working with dangerous pathogens how do we make sure they don’t get infected? And there also have legal questions about how much that ought to be required, and similarly something that I would love to see people work on, is also figuring out if there are safety requirements that we are requiring of scientists today that actually aren’t that useful.
Because I know a lot of scientists find these types of requirements really onerous, and so on the one hand, we really want to eliminate the chance of any accidents. On the other hand, we want to make it as easy as possible for scientists to comply, so we really want to make sure that we’re only asking for things that are valuable so we can really build up a culture of safety among scientists who work with dangerous pathogens.
Robert Wiblin: So it sounds like there’s a lot of things there, a lot of different opportunities because there’s so many different angles on the problem. Preventing, detecting it early, responding. It seems like there’s dozens of potential interventions.
Howie Lempel: I think that there’s a lot of work to do, a lot of work for people from different fields. Something else that I just ought to mention is I think that there’s a lot of really important social science to be done too. We’ve talked about how the problem of nonproliferation becomes much more difficult and maybe in some ways almost impossible, if you don’t even need to bring an actual physical organism from one place to another if we end up in a world where progress is faster than expected and you can just have a desktop synthesizer and create a new organism. There’s not much of a way to screen for that. So what you’re really going to need there is ways to think about how do you build a culture of security so that people are less likely to misuse this technology?
Are there things that you can do to get the DIY bio community to really look out for each other and notice if somebody’s doing something unsafe or doesn’t have good security practices? And figuring out what motivates people to actually really focus on safety and security, which can feel like a chore, I think is a really important problem. Megan Palmer is a social scientist and biologist at Stanford who’s working these types of issues, but I think that there aren’t nearly enough people working on this type of thing.
Robert Wiblin: Right. When you described the desktop synthesizer and just making all of biology a matter of information that you can spread over the Internet, that sounds pretty concerning to me. Are there things that we ought to be banning or technologies that we should be trying not to develop because we’re just better off not having them?
Howie Lempel: I think that’s a really difficult question. I think something that’s really important is that the technology sounds scary because they’re so powerful, which means that they also can have really enormous benefits. So one big challenge right now, that we would have if we were responding to a really novel pathogen, is that we wouldn’t expect any hospital to have stockpiles of vaccines or diagnostics. In a world where you had like biological 3D printers, you wouldn’t have to have this huge stockpile. You could literally develop a vaccine, email the information to a hospital, and have them print it out on the spot. So it’s certainly possible that there are technologies that we shouldn’t develop.
I am both really wary of doing that type of stuff … I think a lot of the biggest gains that society has ever seen come from bioscience. And I’m also a little bit skeptical of the possibility. I think for most really powerful technologies, someone somewhere is going to develop it, and if you push it underground there are risks there too. So for the really broadly useful technologies like advances in synthesis … It’s hard for me to imagine a world where banning that type of thing is both useful and successful. There are types of science that are specifically at the most dangerous end where there has been more dialogue about whether there should be restrictions.
The best example there is those experiments we talked about earlier, where … So gain of function research, where you take a virus and modify it to make it more dangerous, and there’s been a real debate in Washington both about whether or not scientists ought to have to get approval from the government to do that type of work, and whether it ought to happen at all, whether they ought to have to show big enough benefits before they do that type of work. I think that that’s a really important debate. Also on whether or not the results on that type of work ought to be public. So that strikes me as a really important debate, and I think that at least for gain of function research that creates potentially pandemic pathogens, there ought to be a pretty high barrier for how much of a chance of a benefit you have to share for the research before people work with something that risky.
Robert Wiblin: So what kind of reforms are needed at the international level? We discussed some earlier but are there other changes that you’d like to see?
Howie Lempel: I definitely can’t be comprehensive there because I think the answer is that there are a lot of things that could be improved. So one big one, as we talked about, is having some type of coordination around response, and whether it be the WHO or some other organization, we’d like to seek to have a system so that if there is an outbreak everybody knows who’s responsible and has the resources automatically in place. I think that’s one really important goal. A second one is you probably do need some international coordination on research and development into the types of what we call medical countermeasures, which are diagnostics, and treatments, and vaccines that would be useful in sort of low probability, high-impacting areas.
Because these scenarios are both low probability and could happen anywhere and would affect the whole globe, there’s sort of an under-incentive for any individual country to put in the research to work on them. So I think some type of additional coordination on researching those in advance would be incredibly useful. And you can imagine, treaties are like institutions that different countries contribute to, they’re doing that type of research. You really want some type of nonproliferation regime and agreements on what types of pathogens or technology are dangerous enough that there should be restrictions about who gets to use them, and who gets to export them, and that type of thing.
We’d like to see a lot more just resources going from rich countries to all different aspects of this problem. And then a sort of area that I think is really important is just have people even do really pie-in-the-sky theoretical research on the question of, if we had a worst-case scenario, what parts of the system that we currently have in place to address epidemics in general would do a bad job of handling that type of scenario? The types of things that could really lead to a big global catastrophe might be something that’s infectious for a really long time before somebody starts getting symptoms, which slows down the response, and means that by the time there’s a response the initial infected person could have spread the disease really far. Something that I’d be really interested in seeing people work on, is asking: are there ways to catch that type of outbreak in advance? Because that’s the type of thing that’s really neglected because it will only be applicable in these types of scenarios, but those are the scenarios we gotta be most worried about.
Robert Wiblin: So that’s the incubation period, right?
Howie Lempel: Yes.
Robert Wiblin: I guess HIV is a great example of this, right?
Howie Lempel: Yes.
Robert Wiblin: HIV is actually extremely non-contagious in a way. It’s actually not easy to transmit at all, but the incubation period is so long, and the person survives for so long that there’s many opportunities for them to pass it from one person to another which has made it spread reasonably well.
Howie Lempel: Yes. I think thinking of creative ways to notice outbreaks like that much earlier than we do now is really important. You can think about similar issues on the diagnostics and vaccines side. So if we’re talking about the types of diseases that people get frequently on a day-to-day basis that are endemic to a particular area, the current diagnostic system where you take a guess at what the person probably has and just test for it, works reasonably well. But we’re not most likely to get a global catastrophe from the types of things that we’ve seen before. If we really have a global catastrophe, it will probably be from the type of pathogen that we haven’t faced before.
So thinking about broad-based diagnostics that would be able to give us information even about pathogens that are novel, or platforms for manufacturing or developing vaccines really quickly based just on the sequence of a pathogen that we didn’t know much about before, those are areas that are really important from the perspective of somebody who cares a ton about minimizing the risk of a global catastrophe that might be neglected by people whose job is really to protect a specific country from the risks that are most likely over the next years.
Robert Wiblin: These international reforms I guess could be pursued in departments of foreign affairs or State Department or potentially the military to some extent, or you could try to become an elected politician, or go into international bodies like the World Health Organization, OECD perhaps, the United Nations or the relevant bodies in their relevant agencies. Which governments do you think matter the most? Obviously, the United States is a big player. I guess China is also an important one. There are probably not many listeners that are able to get into the Chinese government, but if you, maybe think about that. I guess there’s also the UK. Any others that we should be thinking about?
Howie Lempel: Yes, I think you hit some of the major ones. The United States puts a lot of resources into the issue so there’s a lot of leverage from working there. Countries with emerging biotechnology industries might be really important, so China is a really good example there. India is another good example there. And then, I think it’s also worth emphasizing that government isn’t the only place to do this type of work. So I often compare the nuclear security industry to the biological security industry. In the nuclear area, we have a lot of advocacy organizations; Ploughshares and the Nuclear Threat Initiative are two out of many examples, and you don’t have as much of an advocacy sector in the biological threat pandemic area. So I think being at a nonprofit that was able to really push government and put up a fuss when government neglected these issues, I think would be really important.
And then for a lot of these issues, I think we don’t even know what the right policy is yet, and so sort of think thank an academic policy research, just trying to figure out what the cost benefits would be of different regulatory approaches and of different coordination mechanisms, and talking to a lot of doctors and scientists to figure out what would be the most beneficial arrangements that would have the least onerous impacts on the scientists and doctors who are doing their jobs, it would also be incredibly valuable.
Robert Wiblin: So what kind of improvements to security protocols are needed in your view?
Howie Lempel: I mentioned a few of them but I think that one of the main ones is thinking about this area of nonproliferation and as it becomes more and more possible to modify organisms, and realizing that the approach where there is a specific list of pathogens that you can’t export is no longer going to work, so really over time adopting those types of agreements, I think is really important from a security perspective. A second one is finding ways to both detect any type of use of biological weapons as quickly as possible and also have law enforcement really trained on how to deal with these issues. I think both of those are incredibly important. The United States has some programs aimed at detection where they’ll have sensors in the environment that are supposed to pick up pathogens in the atmosphere. Most people are not very optimistic about how much of a success that’s been so far. But I think that that type of thing is incredibly important.
I think also there have been a bunch of policy simulations done where they did tabletop scenario testing with politicians to see how they would respond in the case of the use of biological weapons. I think one of the lessons from that is that there isn’t really a ton of knowledge about what the process would be, how it would look different from the response to a natural outbreak, so really having some planning and training about what response ought to look like. And then I think it’s really important to just work closely with the communities who are involved with and using this technology, and figure out whether or not there are ways that policymakers could support them. They all want to make sure that their technology is used in a secure way, and they’re talking to them about how to build a good relationship between the people who are doing the security work and the people who are doing the actual science I think is really important. And just in general, I think a lot of thought needs to be put into what security ought to look like.
Robert Wiblin: Are there any technologies specifically that you’d like to see developed? You mentioned one just then but is there anything that entrepreneurs, or academics, or engineers could be working on that would be helpful here?
Howie Lempel: Yes, I think that there are a bunch of areas. I am not a scientist so I think a lot of people might be able to come up with things that I haven’t even thought of yet, but some areas that I think people could do a lot of good; one of them is in the area of countermeasures. So designing diagnostics that would function well in a world where we’re facing novel pathogens as opposed to pathogens that we already know about. Designing a way care diagnostics, so diagnostics that a doctor could just use on the spot and immediately get results, as opposed to diagnostics where you have to take a sample and then send them to a lab to then analyze, which can be way too slow in a crisis. Thinking about platforms for rapidly designing vaccines and treatments that are broad-based enough that they can function for multiple different pathogens that might be useful if we saw something new.
So I think all of those are really important areas, and we talked a little about things like designing biosafety measures that could be baked into synthetic biology. So biology’s thinking about ways to make it really easy to design a synthetic organism that wouldn’t be able to survive if there was an accident in the environment. I think that that’s really important, and then I think that there’s a lot of work to be done on the surveillance side too. So thinking about technologies that could help us notice a outbreak more quickly, like is there a way to work with … Google did some really interesting work called “Flu Trends,” where they analyzed people’s searches and were able to use search data to notice flu outbreaks about at the pace that the CDC was noticing them.
Robert Wiblin: That stopped working, right?
Howie Lempel: Yes. That didn’t work in the long run, but I think that there’s a lot stuff in that realm where there’s data out there that we don’t know how to make use of. So, is there anything that we could do with electronic health records, so that if we had more people than usual showing up to a hospital in the local area people can notice sooner? So I think that there’s a lot of potential for innovations in that area.
Robert Wiblin: It sounds like you’re more into surveillance maybe than prevention or treatment. Is that just more what you know about? Or do you think that that is perhaps the highest leverage thing to lean on?
Howie Lempel: I think I’m actually pretty agnostic. Yes, I would say I’m pretty agnostic about that. On the prevention side, all the nonproliferation stuff I think of as prevention, and I think that that’s incredibly important. And then on the treatment side, I think that I might be … This is just my intuition I don’t have a ton of confidence on. I might be a little skeptical of the ability to just as an individual, expand the quality of treatment and response given current technology, because I just think that there are so many different places where an outbreak could occur, that it’s pretty tough to know exactly where are the most valuable places and what’s most neglected there. But I think there’s a lot of research that could be really important on the response side. So all of this stuff around researching diagnostics and countermeasures in the response area, I think that that can be really vital. And I think there’s a lot of room for policy advocacy on the response side too.
Robert Wiblin: On prevention, what about trying to stop humans from having contact with wild animals? Is that something that anyone is actually trying to do?
Howie Lempel: There’s a little bit of work on that, and the name of a couple of the organizations I know that work on that, it’s escaping me. One of them is called the Eco Health Alliance, actually, but there are a couple of other organizations that have done some work on that. It strikes me as something that I would love to see more of. I guess my personal intuition is that it doesn’t strike me as the highest leverage thing to work on for a few reasons. One of them is that it’s almost exclusively focused on the natural outbreak problem, and because I think that there’s a potential for man-made outbreaks to be even higher impact, I’m a little bit more optimistic about interventions that would be useful for those scenarios or in both scenarios.
A second reason is that even if you improve techniques for handling wild animals, you also need to find a way to get them implemented and I think that that’s a really difficult problem, because it requires changing the behavior of just a really large number of people. There can be cultural barriers there, it can be difficult to scale that and have the communication necessary, and then for each different animal population there are probably going to be different techniques, which makes it seem like a little bit less leverage to me. But I know a bunch of people who work in the area who I really respect, who disagree with me and think that this ought to be a priority. So yes, don’t totally take my word for it.
Robert Wiblin: Sure. On the treatment side, what about developing a lot of slack vaccine production capacity? So we can very quickly scale up production or we have a lot of vaccine research scientists waiting around, maybe doing something that’s not that useful right now but they’re ready to step into action when we need them to.
Howie Lempel: Those both strike me as very good ideas that I’d really like to see happen. My concern with both of them is about whether or not they would be sustainable, especially politically. So if you have all this slack vaccine capacity, there’s just going to be the question of how you keep it slack, and I think that you might be able to keep it that way for a little while, but eventually you’ll have a minor outbreak of a common disease. I think people will react against the fact that you had slack that wasn’t used, and eventually policymakers are going to say, “What are we doing leaving this open?” So to me, what seems most promising is more risky blue sky research into ways to just lower the amount of time that it takes in the first place to manufacture vaccines and countermeasures. I think that that’s going to be probably where the big gain will come from.
Robert Wiblin: Perhaps the ability to quickly redesign from the same facility so it can switch from producing one thing to another?
Howie Lempel: I think that that type of thing would be really valuable.
Robert Wiblin: So, thinking now about what people listening to this could concretely do, someone who’s listening to this and they’re convinced that this is a serious problem, something that they would like to help with, what should they study now perhaps if they’re young and choosing their major, or maybe what should they do a PhD in?
Howie Lempel: Yes, so one that I think is pretty unique about this field is how interdisciplinary it is. So there’s a lot of important social science to be done in policy research. There are defense and diplomacy and military aspects, there’s hard science biology and microbiology aspects, there’s tech and entrepreneurial aspects, and then there’s also medical science aspects. So there are, I think a lot of promising avenues for what one might study and what background someone might want to have, and I can talk through one of those. But I would say that one thing is you want to have at least some background in biology, something that I don’t really have and wish I did. So I think that that’s definitely something that someone would want to focus on.
And I think that as we go forward, it’s possible that synthetic biology in particular has a chance of being a really important technology, that both might be associated with a bunch of risks and also might be really promising for things like developing countermeasures quickly. So I think having a background in that area could be really valuable, but there’s plenty of work to be done for people who don’t have that background. And then something I think is a big gap in the field, is because of the way that academia is siloed, and also, most of the work at government agencies is like siloed within a particular agency.
You have this problem where it’s a really interdisciplinary area, but most people are specialists in that particular area, so I think having people who have a broad background in several of the required areas is incredibly important. So it can be tough when I ask someone whose whole career has been in developing surveillance so that hospitals notice more quickly, or ministries of health notice more quickly when there is an outbreak, and ask them, “What would you love to see change about the way that vaccines are developed?” They really don’t have the breadth to really know, and I think especially policymakers really need to have that type of breadth.
So I think whatever specialty that people go in, having some really intentional efforts to network broadly in the community and get to know colleagues in neighboring areas is really important. So I guess to be a little more concrete about specific areas that people could go in, one of the major possibilities is to look into epidemiology, studying how to forecast once an outbreak occurs how serious it will be, looking into the effectiveness of different types of containment measures. Epidemiologists are also often the first ones who arrive when an outbreak has been detected but nobody knows what the pathogen is yet, or how many people have been infected.
The CDC has a program with a really great reputation, where they train field epidemiologists to go around the globe and to be these first people or sort of disease detectives. I think going and getting training, getting a PhD in epidemiology, could be really valuable. I think it will also be useful for people who might care in particular about risks from biological accidents. We really need some people who care about that issue, but are epidemiologists and can do this sort of cost-benefit to say if a certain type of pathogen were released, how risky is that exactly. So people who are mostly microbiologists, their specialty isn’t always on the macro health issues, like how will people react to this, and how fast will it spread, and how many people do we think will get infected. I think that that’s a really important area.
There are various really great PhD programs in epidemiology, and I can’t list them all here. Someone who’s working in any of these areas really ought to get some advice and mentorship from somebody who’s an expert but there’s been some really great work done by Marc Lipsitch on some of these issues who’s a epidemiologist at Harvard’s public health school. And then the center for health security is a think tank at Hopkins that was given a grant by my old employer, Open Philanthropy, that has some researchers who work on those types of issues. So I think connecting with those folks would be a really great way to work in the field, could both be a potential job for somebody who wanted to work in the field and also might make Hopkins a really attractive place to study epidemiology.
There are other paths in microbiology and synthetic biology and really getting involved in that type of technology and thinking about ways to innovate and make sure it’s safe, make sure it’s secure, and also find innovative medical uses for it. Harvard is a great place to do that type of work too. Stanford is also. George Church at Harvard is a top synthetic biologist who also has worked a bunch on safety and security issues, who’s thought a little bit about ways to really change the technology to build safety mechanisms into it.
Robert Wiblin: George Church was involved in the development of CRISPR, is that right?
Howie Lempel: Yes, that’s right.
Robert Wiblin: Okay.
Howie Lempel: And Drew Endy and Megan Palmer at Stanford are both really great experts on synthetic biology who have thought a bunch about safety and security issues. Megan Palmer, in particular, has thought a bunch about the social science and working on building a culture of safety and security and what that looks like. And then there’s … You’d have a more medical and health research focus, than traditionally if you were going to go work on pharmaceuticals or vaccines or diagnostics. You might get a MD and biology PhD dual degree. I’m not really an expert in the best schools to go to for that, but I think the things that you want to look for are both going to a highly ranked school that will give you a lot of options, and making sure that there are mentors there who share some of these interests and can help you get integrated into the field.
And then secondarily, I think it would be a good idea if possible to look at the departments you’re not studying in, and see if there would be opportunities to collaborate with people in neighboring fields, who also work on these issues. So I think being somebody who’s getting an MD but is collaborating a lot with synthetic biologists, I think would be really, really valuable.
Robert Wiblin: So we got medicine, biology, synthetic biology, bioengineering, social science, economics, international relations, politics. It’s like a very wide range-
Howie Lempel: Yes, there’s some specific defense programs that focus on biological security. I think that King’s College has one, although I’m not positive I’m getting that right, so I think that that would be something to look into also. There’s a professor at Columbia, Jeffrey Shaman, who’s working a lot on disease forecasting, and trying to ask: how quickly, once we know about an outbreak can be try and forecast where it will spread to kind of guide their response.
Robert Wiblin: So we’d be asking what are the leading indicators and how it’s going to go? So what things can we see in the first week that will-
Howie Lempel: Trying to use actually techniques from weather forecasting, and seeing if we can use that to forecast the spread of an epidemic. That would be really valuable for resource allocation during the response.
Robert Wiblin: So you’ve just added security studies and military work and I guess also data science? Potentially machine learning also come into it? So there’s just an enormous range of potential. Yes, areas of expertise that could be relevant.
Howie Lempel: Yes. That’s right.
Robert Wiblin: It seems like yes, this problem is very unusual in having a very large surface area. There’s lots of places where you can start trying to get to grips with it and making a difference.
Howie Lempel: Yes, I think that’s definitely right.
Robert Wiblin: Yes, I guess especially compared to say, to nuclear security, another catastrophic risk where it seems like if you’re not part of one of the relevant countries and you can’t get into the decision-making apparatus there, then you’re somewhat cut out of the situation.
Howie Lempel: Yes, and it’s pretty centralized. I know a little bit about the nuclear security industry and there’s a pretty small set of programs where most of the experts all come from, and the community is very well-organized and has a lot of methods for collaboration. That’s less true for biosecurity, which means it’s a pretty big diversity of paths someone can take. I’ll mention that one opportunity that Open Philanthropy has funded that I think might be really valuable for early career professionals in the area, is the Emerging Leaders in Biosecurity Program, which is run by the Center for Health Security and selects fellows to take a few days a couple times a year to go to meetings where they all meet each other.
It’s a networking opportunity, they get introduced to tons of experts and they are able to really have an opportunity to talk to and collaborate with people from other fields who are also interested in biosecurity. I think that that’s both a really valuable program for people to potentially apply to once they’re working in the field, and it’s also a good way to just see a list of different people who are all working in the field, and see the types of opportunities that are out there.
Robert Wiblin: So you’ve listed quite a few places to study and some potential PhD supervisor people could speak to. I don’t want to stop you if you want to list anymore. Is there anyone else or anywhere else that you wanted to get out there for people to look at?
Howie Lempel: I think thinking about MIT’s synthetic biology program would be another place to look into-
Robert Wiblin: Do you know any specific people there who are …
Howie Lempel: Yes, Kevin Esvelt is a young researcher who’s worked a lot on gene drives and synthetic biology, and also is really interested in safety and security issues. He might be an interesting person to work with. Joe DeRisi at UCSF is a synthetic biologist who’s worked a bunch on security issues, and also on medical issues, and could be someone really interesting to work with. Berkeley also has a really great synthetic bio and genetic engineering program, so there are a lot of options there. And then a few medical schools that really do focus on these types of issues that might be good places to go, especially if you’re interested in doing something like actually being actively involved in on-the-ground response; University of Nebraska and Omaha is one of the places where a lot of the people of the Americans who got Ebola and then got sent back to the United States were treated.
They have a real focus on rare infectious diseases and do a lot of work training people internationally and how to respond to them. Emory is another really good school for those types of issues, I think in part because it’s in Atlanta and it’s also where the CDC is based. So there’s a lot of crossover where professors of Emory will also work with the CDC on projects.
Robert Wiblin: And those are medical schools?
Howie Lempel: Those are medical schools. Also public health at the University of Nebraska.
Robert Wiblin: Okay. Well, I’ll see if I can compile all of those into a list that people can scan through if they’re looking for potential places to study in the episode notes. So once you’ve studied and perhaps you’ve done a PhD, what are some smart early career steps? How do you go about building a network perhaps and learning other relevant skills that would really allow you to make a difference? I guess one thing you suggested is trying to be interdisciplinary.
Howie Lempel: Yes, so I will give you some thoughts. I will also add that I did not have a career in this field, so I can talk about know what some of the people I’ve interacted with seemed to have done, but I think the best piece of advice I can give is to really don’t be shy about reaching out to people who have the type of career that you would like to have, and getting their advice and seeing what they did. But some types of things that people tend to do when there’s a lot of opportunities in both the tech and pharmaceutical industry to work on vaccine development. Then there is a lot of areas in the government, and because there’s no existing market that PhRMA companies can count on, that will necessarily buy vaccines that are only going to be useful in a crisis, it means that a lot of the work happens in governments or is funded by governments. So there are parts of the NIH that work on this. DARPA and IARPA both think a lot about biosecurity and about risks from emerging diseases. BARDA in the Department of Health and Homeland Security-
Robert Wiblin: What’s BARDA?
Howie Lempel: So they are the Biomedical Advanced Research Development Agency, I want to say is what the acronym stands for, but it’s part of the Health and Human Services Department in the United States that specifically works on trying to help medical countermeasures that would be useful in outbreaks get from the very early stage research into development. So they pick up and subsidize and work with companies to do that type of translational research, and often have some role in helping to set priorities for what types of research in this area the US government will fund.
Robert Wiblin: Do you see much opportunity for people to contribute through entrepreneurships? So starting their own for-profits or perhaps nonprofits?
Howie Lempel: Yes, I think that there’s a lot of room there, especially that’s on the innovation front, so I think that there are not enough people trying really blue sky risky ideas for research that could lead to systems that would let us develop countermeasures really quickly from novel pathogens. And I think there’s a lot of room in biotech for people to do that type of work, so yes, I think that that would be a really good opportunity for a lot of folks.
Robert Wiblin: Yes, so in terms of building a network and getting to know these people, we should just email them? Is that how to go about it? Or is there conferences perhaps that you could go to where people could meet people who are doing the relevant epidemiology or the relevant medical science?
Howie Lempel: There are a couple of main conferences and they are slipping my mind at the moment so we can maybe put them up in the links later. So I think that going to conferences is one opportunity. The Emerging Leaders in Biosecurity Program, I think is another main convening area. A difficulty is that because the disciplines are so siloed, there’s often different conferences for each discipline, which makes it a little harder to network in this field. The CDC also has some training programs that I think would be really good ways to get involved in the field. A lot of people start out in their field epidemiology training program, and I think that that’s a good way to build a network too.
Robert Wiblin: And that’s just called the CDC Training Program?
Howie Lempel: It’s the CDC Field Epidemiologist Training Program.
Robert Wiblin: So we’ve mentioned a whole lot of different labs and organizations over the last few hours. Are there any agencies or organizations you would particularly like to highlight that you think would be good places for people to go work early in their career?
Howie Lempel: Yes, some of them I mentioned already but the Center For Health Security is a big one. It’s a think tank. It’s one of the few think tanks that’s really focused entirely on these issues. IARPA and DARPA I think are two of the branches of the US government that are willing to fund really risky research on this type of area and have the latitude to do that, so I think that those could potentially be really good career paths. DTRA, the Defense Threat Reduction Agency at the defense department, is one of the main sites of the defense department that works on preventing the use of weapons of mass destruction, and I think that that would be a really good launching off point. So those are several ideas, but I think that there really are a lot of ways to enter this field.
Robert Wiblin: So looking a bit more-
Howie Lempel: Also working in Congress, I think is another …
Robert Wiblin: Yes. I was going to say looking a bit more broadly, are there positions for journalists? Any particular journals or newspapers you could look at that are covering this, looking like nothing in particular?
Howie Lempel: I think it would be incredibly valuable for that to exist, but I don’t know that there is sort of … I think you would have to create your own job which strikes me as totally plausible. Vice did a particularly great series on outbreak prevention, but it doesn’t mean that they’re looking to hire a bunch of full-time journalist to work on this type of stuff. But it’s at least a place to go for an example of some really good journalism on this issue.
Robert Wiblin: Yes. So you mentioned working in Congress. You’re thinking as a Congressional research staffer or like …
Howie Lempel: Yes, as a staffer I think on a committee seems like there’s at least a lot of potential to have a big impact there. There’s a lot of areas of US law where I think you really can make a big impact.
Robert Wiblin: What about relevant committees? Do you know if-
Howie Lempel: I’d have to get back to you on that.
Robert Wiblin: Yes, sure. No problem. What about think tanks? Are there any think tanks that are doing research in this area? I think Brookings has a bit, maybe Chatham House in the UK I think has a program…
Howie Lempel: Yes, Chatham House does. Brookings might have a bit but I think it’s less. The Center for Health Security is a big one. It’s not a think tank exactly, but there’s an academic center at Georgetown that’s relatively new. Run by two researchers; Rebecca Katz and Julie Fisher, I can’t remember what it’s named but that’s another organization that Open Philanthropy funds, that does policy research that’s think tank-ish. I think that the main place I’ll point to are Chatham House and the Center of Health Security.
Robert Wiblin: I guess any group that OpenPhil is funding this area is probably also promising…
Howie Lempel: Yes, I think that will be a good way, yes.
Robert Wiblin: I’ll put up a link to all of the grants that OpenPhil has made in this area so people can explore.
Howie Lempel: That’s a good idea.
Robert Wiblin: And also, just fishing, are there any startups? Any biotech startups that are doing particularly impressive work that come to mind?
Howie Lempel: Nothing that I could name off the top of my head.
Robert Wiblin: Yes, sure. One thing that people often think about when they’re considering going into a somewhat niche area like this is, what if they change their minds while they’re doing their PhD or their life circumstances change and they want to move into another field? Are people who are in this developing really transferable skills that they could then apply more broadly to other areas? Or are they going to end up a little bit locked in?
Howie Lempel: I think it depends on exactly what they’ve specialized on, and on how much of a transition you want to make. People in this area are often really well-positioned to work on biotech more broadly, other medical or health issues. If you want to work on global public health and poverty alleviation, I think there are sometimes opportunities to transfer in that direction. If you work on the security side, working on other security-related issues seems like a possibility. So I think that there are opportunities out there for people with biological, and medical, and security and policy backgrounds. If somebody wants to transfer into something totally different, go work in consulting and finance afterwards. It’s not like you’ll have a limited opportunity but you’ll probably have sunk some time into it.
Robert Wiblin: Yes, but they’re all pretty respectable fields. There’s a lot of different aspects to them so you’re probably not going to end up on the streets. What are the signs that working in this area is a good fit for someone? Are there any indicators? I suppose there are so many different angles, that it’s a bit hard to make generalizations about this-
Howie Lempel: Yes, I think that’s the main thing, I would say. I think there’s a particular need for people who are good biologists, good microbiologists, so I think that’s one area. Another area is people who are interested in the intersection of health and security are pretty rare. People tend to either be interested in public health or in security so if you’re interested in and have a background in both of those, I think that could be a good sign. And then there’s I think a lot of difficulties because it’s such a siloed field with communication. So if you realize that you feel really at home among people who are interested in military issues, interested in security issues or law enforcement, and also among biologists and scientists or health-oriented people, that also seems like a good sign.
Robert Wiblin: Well, you’ve given us so much time here and so much information. Is there anything I should have asked that I haven’t asked?
Howie Lempel: Nothing that I have in mind but you should feel free to follow-up over email if anything else comes up.
Robert Wiblin: Do you want to have a final call to arms to people? Inspire them to go forth and solve this risk that we all face?
Howie Lempel: Yes, I’ll do my best. I truthfully think it’s one of the most important issues for people to think about if they’re concerned about the long run future. I think that Bill Gates is right to say that if tens of millions of more people are going to die in an event over the next few decades, and this is one of the risks that’s most likely to cause it, and then it’s a really, I think, exciting area, because there are so many open questions and it’s just so easy to point to areas where nobody knows what the best policy is, but gee, it really seems important if this technology is developed that somebody will figure it out. There have been a lot of progress in developing vaccines, but it’s really important that we also be thinking about vaccines that would be useful for novel pathogens that we’ve never seen before.
I think that there’s just a lot of really interesting opportunities for people to do a lot of good. I think a lot of the areas that seem neglected in other spaces, it feels like a bit of a challenge to take on because the reason that they’re neglected, is nobody even knows what type of research would be useful. And it’s something really, I think exciting about that pandemic preparedness and biosecurity area. I think that there are a lot of really concrete opportunities to do a lot of good work that maybe aren’t focused on because there are similar opportunities with more funding or more attention on more traditional public health issues. So yes, I think it’s a really interesting area to work on and people should go for it.
Robert Wiblin: My guest today has been Howie Lempel. Thanks for coming on the 80,000 Hours podcast.
Howie Lempel: Thanks Rob.
Related episodes
About the show
The 80,000 Hours Podcast features unusually in-depth conversations about the world's most pressing problems and how you can use your career to solve them. We invite guests pursuing a wide range of career paths — from academics and activists to entrepreneurs and policymakers — to analyse the case for and against working on different issues and which approaches are best for solving them.
Get in touch with feedback or guest suggestions by emailing [email protected].
What should I listen to first?
We've carefully selected 10 episodes we think it could make sense to listen to first, on a separate podcast feed:
Check out 'Effective Altruism: An Introduction'
Subscribe here, or anywhere you get podcasts:
If you're new, see the podcast homepage for ideas on where to start, or browse our full episode archive.